Laparoscopy for Trauma
Kenneth J. Ransom, MD, R. Stephen Smith, MD
INTRODUCTION
The use of laparoscopy in the management of trauma patients continues to be limited. Although reports of laparoscopy for the diagnosis of traumatic hemoperitoneum date back to the 1920s, its applications have not grown at the rate observed with other general surgical diseases.1,2 Villavicencio reviewed the world literature in 1999 and identified only 62 significant publications related to laparoscopy for trauma.3
Many trauma patients are not candidates for minimally invasive surgery due to hemodynamic instability or complexity of injuries. Control of life-threatening, complex intraabdominal injuries requires rapid exposure of the organs that can only be accomplished through an open celiotomy incision. The time required to set up and perform a laparoscopic procedure along with the limited exposure makes laparoscopy an unrealistic option in the critically injured patient.
Associated extraabdominal injuries may also preclude the use of minimally invasive surgery. Josephs et al and Rosenthal et al demonstrated increased intracranial pressure in animal head-injury models with insufflation of the abdominal cavity with CO2, and Mobbs reported on the dangers of laparoscopy in head-injured patients.4,5,6 A “gasless” technique has been described by Smith to primarily avoid the potential complications of CO2 insufflation: intracranial hypertension associated with head injuries, air embolism, and the development of a tension pneumothoraces in cases of occult diaphragmatic injuries.7 This technique however does require special equipment and limits exposure to only one quadrant at a time.
Laparoscopy and other minimally invasive surgical techniques can be applied when a primarily intraabdominal injury is suspected in a hemodynamically stable patient.
Hemodynamic stability sufficient to consider laparoscopy in the trauma patient was defined by Choi and Lim as a systolic blood pressure >100 mmHg and diastolic >60 mmHg, a heart rate <110 beats per minute, and crystalloid resuscitation requirements of <2 L.8
Laparoscopy can be used alone or as an adjunct to other diagnostic modalities to determine the presence of an intraabdominal injury. These include diagnostic peritoneal lavage (DPL), focused abdominal sonography for trauma (FAST), and computerized tomography (CT) of the abdomen.9,10 DPL is very sensitive for peritoneal penetration and specific for visceral injury with intraperitoneal spillage of enteric material.11,12 Laparoscopy was found in a comparative study to also be highly sensitive, but more specific and accurate than DPL. FAST is less sensitive and specific than DPL but is very fast and noninvasive.13 CT scan is less sensitive for peritoneal penetration and visceral injury but provides much more information about solid organ and retroperitoneal injuries.14,15
The first reported application of modern laparoscopic techniques for diagnostic purposes in traumatic injuries was by Gazzaniga in 1976.16 He reported on 13 patients with penetrating injuries and 24 with blunt trauma. Interest and comfort with laparoscopy in trauma has continued to be primarily in its use as a diagnostic tool. Many studies from major trauma facilities reported since the 1970s have supported the diagnostic utility of laparoscopy in select stable patients with both penetrating and blunt trauma.3,13,17-21
Laparoscopy has been shown to be very effective in determining whether violation of the peritoneal cavity by tangential wounds has occurred. In many cases, laparoscopic examination can reliably rule out a significant intraabdominal injury in patients with equivocal abdominal examination following blunt or penetrating trauma. Diagnostic laparoscopy for trauma has been shown to be effective in preventing negative laparotomy in 21% to 59% of patients,16,17,20-23 which can be associated with significant morbidity.24-26 However, the non-therapeutic laparotomy rate after laparoscopy positive for peritoneal penetration of up to 45% remains a concern.27,28Laparoscopy actually has advantages over other diagnostic tests in diagnosing diaphragmatic injury from lower chest and abdominal penetrating wounds29-32 or blunt abdominal trauma.9,18,33 Delayed or missed diagnosis of diaphragmatic injuries are known to be associated with significant morbidity.34
Reports of laparoscopic surgery for therapeutic interventions in trauma patients did not appear in the literature until the 1990s.17,35 Unlike many other therapeutic applications of laparoscopy in general surgery, its use to repair traumatic injuries has been limited.
However, with increasing surgeon experience and improved equipment, the therapeutic applications of minimally invasive surgery in trauma will likely broaden. Choi and Lim recently reported on 65 patients with intraabdominal injuries who underwent definitive procedures performed with minimally invasive surgery including total laparoscopy, laparoscopically assisted (minilaparotomy), and hand-assisted laparoscopy without a single missed injury or major complication.8
PROCEDURE
Minimally invasive abdominal surgery is most commonly used as a diagnostic modality as part of the initial evaluation of hemodynamically stable trauma patients with a possible, primary intraabdominal injury. In most institutions, laparoscopy is performed in the operating room. Reports exist of laparoscopic equipment designed specifically for use in the emergency department environment that do not require insufflation of the abdominal cavity and use of general anesthesia.13,17-19,36 Exposure and visibility are limited however, and its usefulness is strictly as a screening tool. The operating room provides access to more advanced equipment with better visibility and versatility of laparoscopic surgery. In the usual patient undergoing diagnostic laparoscopy after trauma, the standard insufflation technique with the patient under general anesthesia is used.
The Hasson or open technique at the umbilicus is recommended to introduce the initial trocar for insufflation of the abdominal cavity. The insufflation pressure is generally limited to 15 mmHg. Bilateral perirectus 5-mm and 10- or 12-mm trocars, may be added ports as needed. Blood or succus is aspirated and the abdominal cavity is irrigated. Some surgeons will proceed to open the abdomen once they have established peritoneal penetration or that an intraabdominal organ injury has occurred. Others may continue to examine the intraabdominal organs to specifically identify and evaluate the injury to determine whether a formal open therapeutic laparotomy is necessary. Small bleeding sites can be cauterized or ligated allowing for better assessment of the abdominal cavity.
Complete examination of the gastrointestinal track including the stomach and small and large bowel is accomplished by the use of atraumatic grasping forceps introduced through the lateral trocar sites. The anterior wall of the stomach is easily examined for perforations. Visualization of the posterior wall of the stomach requires dividing the gastrocolic ligament and entering the lesser sac. Exposure of the duodenum is more difficult and requires mobilization of the hepatic flexor of the right colon. The anterior portion of the duodenum and portal area can be visualized for an injury or periduodenal hematoma. In the case of a periduodenal hematoma, mobilization of the second and third portion of the duodenum can be accomplished by a Kocher maneuver to assess the posterior wall and head of the pancreas. Exposure of the retroperitoneal portion of the duodenum may be difficult, and only surgeons skilled in working with a laparoscope in this area should attempt it. Conversion to an open exploration should be performed if any uncertainty exists about the existence of a duodenal injury. CT with oral contrast may be another consideration to evaluate the retroperitoneal duodenum.
To examine the small bowel, grasping forceps are used to grasp and elevate 4 inches to 8 inches of small bowel. The next portion is then grasped with a second trocar forceps and “handed off” to the first forceps to elevate and evaluate that segment of bowel. This process is repeated until the entire small bowel and its mesentery have been examined. It is very important that complete examination of the bowel is accomplished to avoid a missed injury.
The intraperitoneal portion of the large bowel is manipulated and examined in a similar fashion to that of the small bowel. Suspicious areas of retroperitoneal bloodstaining observed with the laparoscope or seen on CT scan can be mobilized by retracting the colon medially and dividing the retroperitoneal reflection to visualize the colon.
Portions of intraperitoneal solid organs can be directly visualized with the laparoscope. The posterior portions of the liver and spleen are however not easily seen. A CT scan provides more complete information about the presence and nature of intraabdominal solid organ injuries. Likewise, exposure of retroperitoneum is limited by laparoscopic techniques and accurate diagnostic evaluation is usually dependant on computerized tomography.
Additional ports may be inserted or mini-incisions made to facilitate the examination. Asbun et al reported that hand-assisted laparoscopic exploration is more accurate than laparoscopic exploration alone in detecting injuries (63% vs 38%).37 Choi and Lim placed the patient in a steep Trendelenburg position to achieve better exposure and access to the pelvis and lower one third of the small bowel, supine position for the mid abdomen and middle one third of the small bowel, and reverse Trendelenburg position for the upper abdomen and upper one third of the small bowel.8 They had no missed small bowel injuries in their series. The minimally invasive procedure should be converted to an open laparotomy if a satisfactory examination cannot be accomplished.
Single incision laparoscopy (SIL) is emerging as a less invasive alternative to standard laparoscopic technique. The first SIL cholecystectomy was reported by Navarro in 1997.38 Since then almost every laparoscopic general surgical procedure has been reported using SIL including appendectomy,39 adrenalectomy,40 gastric surgery,41 donor nephrectomy,42 colectomy,43 and prostatectomy.44 The demonstrated access to almost all areas of the abdominal compartment through a single incision site presents certain advantages for the use of this approach in trauma patients. One of the challenges of standard laparoscopic surgery in trauma has been proper placement of the ports. A good port site for one operation may not be optimal for another operation. Usually in trauma patients the injuries are unknown prior to entering the abdomen. Consequently, the initial port placements may not be ideal which may lead to a greater chance of missed injuries. Little if anything has been reported utilizing SIL in trauma patients. As this technique becomes more widely used it will undoubtedly be tried on trauma patients and could potentially demonstrate advantages over the standard laparoscopic approach.
Additional time is required to perform therapeutic procedures on injured organs by minimally invasive surgical techniques. It is essential that the patient is physiologically stable and does not have multiple associated injuries. Important technical considerations for repair or organ removal include quality up-to-date equipment and instrumentation as well as a surgeon skilled in minimally invasive surgery. Hand-assisted techniques may provide better opportunities for exposure and easier specimen removal through greater organ manipulation.8 The operating surgeon should be familiar with hand-assisted laparoscopic surgical principles to properly utilize this technique. Conversion to a mini- laparotomy can enhance safe completion of certain procedures that may require extracorporeal suturing. Preoperative embolization of injured solid organs may provide added hemostasis for a safer laparoscopic operation. Injuries to retroperitoneal organs can be safely managed laparoscopically in select cases. Successful operations on both the pancreas and kidney have been reported following traumatic injury.8,32,45 The combined application of CT imaging with laparoscopic procedures provides new options for managing select retroperitoneal injuries.
COMPLICATIONS
The most common complication associated with diagnostic laparoscopy is missed injuries due to the limited ability to manipulate organs and accomplish adequate exposure.
Studies have shown missed injury rates from 19% to 40%.20-23 Patient positioning described by Choi and Lim and hand-assisted techniques have been shown to reduce the missed injury rate.8.35 Laparoscopic procedure-related complications occur in only 1% of cases similar to that seen with other general surgical applications of minimally invasive surgical techniques.3 These include visceral and vascular injuries from trocar insertion or instrument manipulations.
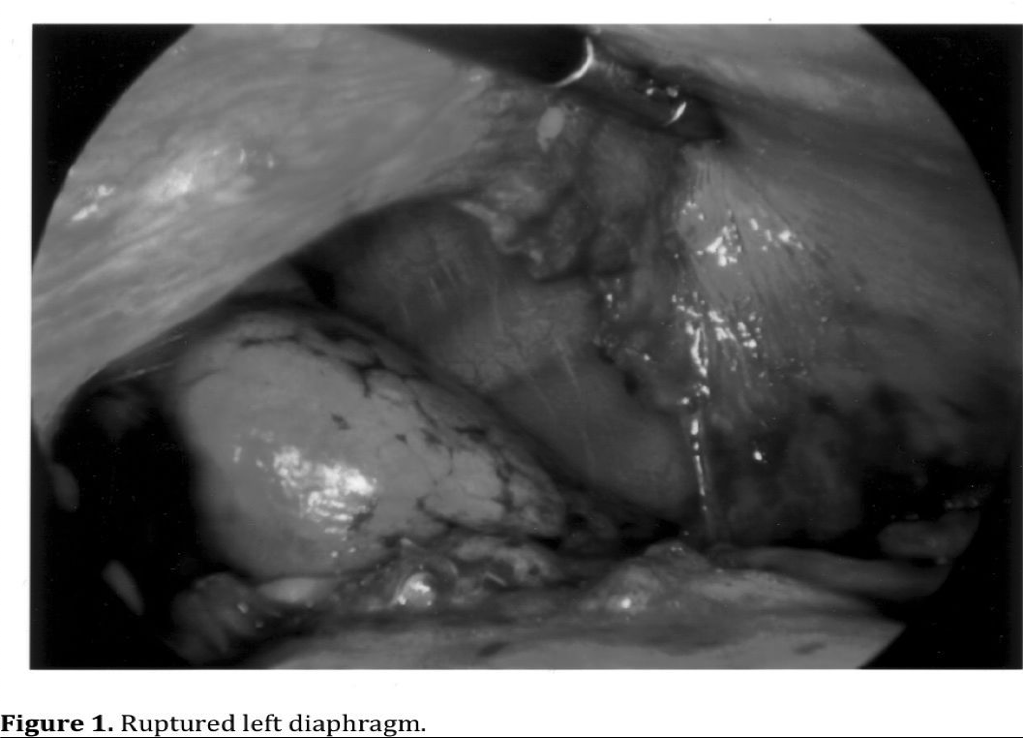
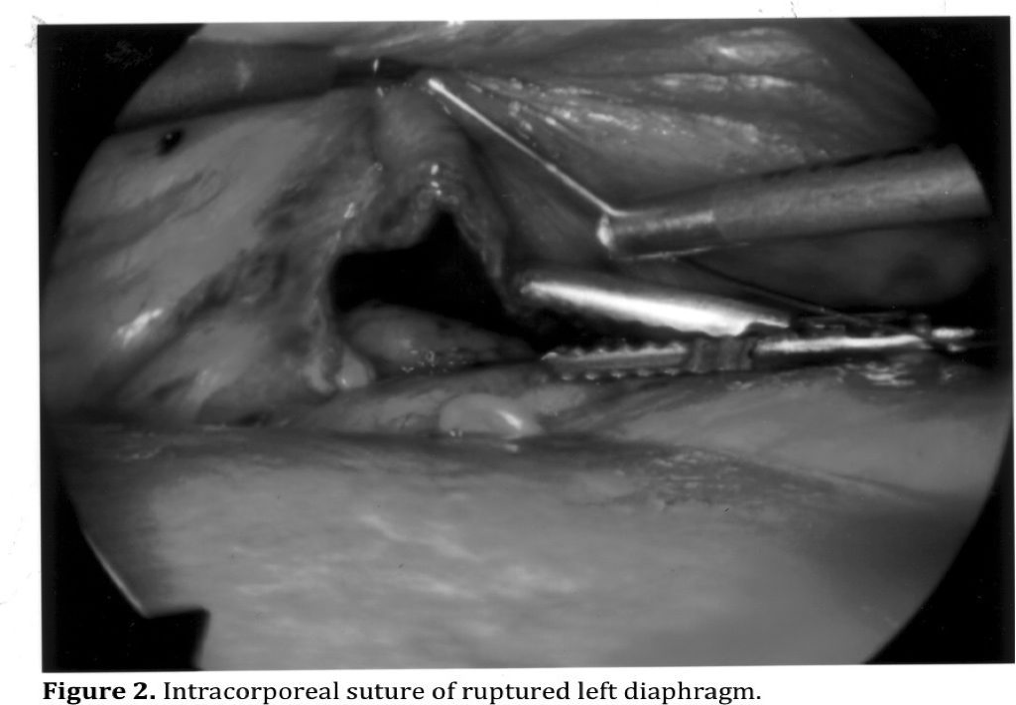
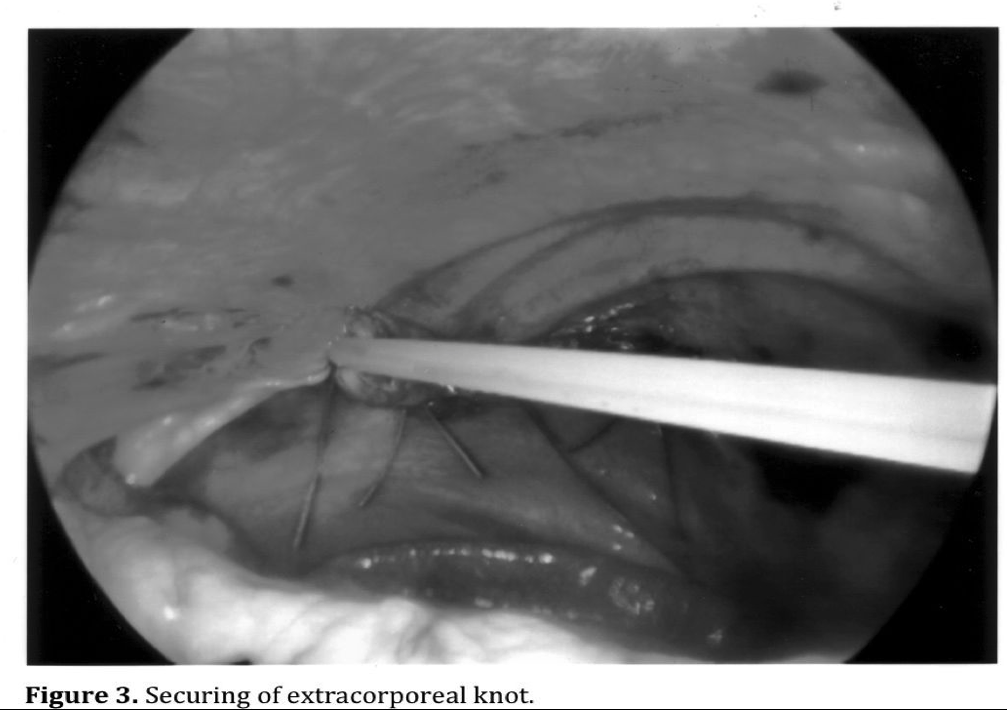
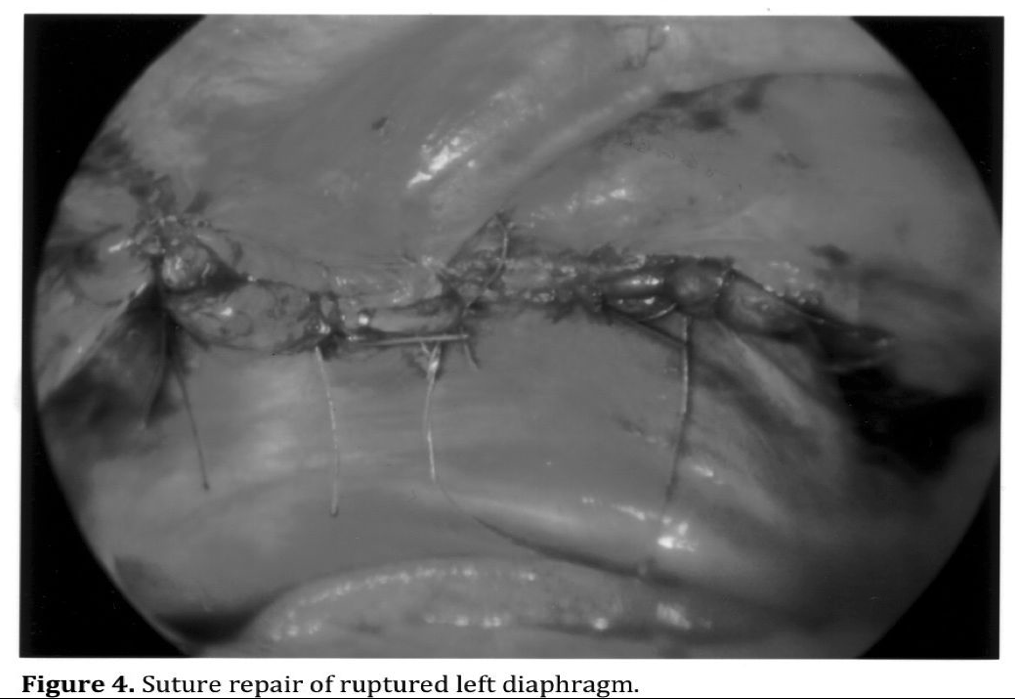
Specific complications are associated with the management of individual injuries. The risk depends on the complexity of the injury being managed. Repair of injuries to the peritoneal wall and diaphragm are the least complicated and most common injuries that can safely be managed with minimally invasive surgery (Figures 1, 2, 3, 4). Exposure is more difficult for posterior diaphragmatic wounds due to patient positioning and organ retraction. It is also important to insert a chest tube in the side of the diaphragmatic injury to prevent the development of a tension pneumothorax from abdominal insuflation.17,29,32
Exposure and suture of bleeding mesenteric lacerations may be difficult and dangerous when near the root in close proximity to major vascular structures. Severe bleeding can result as well as disruption to the blood supply to the bowel when sutures are placed near the root of the mesentery. Management of proximal mesenteric vessels and primary branches can be challenging even with an open abdomen. Minimally invasive surgical repair of mesenteric lacerations should be limited to minor tears that are not near the root.
Solid organ injuries are preferably treated nonoperatively except when the bleeding is severe enough to pose an immediately life-threatening condition, in which case an emergency laparotomy is required. No place exists for minimally invasive surgery in the hemodynamically unstable patient actively bleeding from a liver or spleen injury. Smaller minor anterior injuries of the spleen may be cauterized or topical hemostatic agents may be applied.35,46 Splenectomy can be performed with minimally invasive techniques, possibly hand-assisted, on more extensively damaged spleens following angiographic embolization.8 The presence of a large perisplenic or subcapsular hematoma will make a laparoscopic approach more difficult and dangerous. Small lacerations visualized on the liver may also be cauterized or hemostatic agents applied.17 Combining laparoscopic irrigation and drainage after angiographic embolization may reduce morbidity in select patients with deeper lacerations. The patient should always be properly positioned to quickly open the abdomen when excessive hemorrhage occurs from an injured spleen or liver during minimally invasive surgery.
Injury to the gallbladder may lend itself to laparoscopic cholecystectomy.17,47,48 A cholangiogram should be done when it is safe to assess the remainder of the biliary track for injury. Most injuries to the extrahepatic ductal biliary system cannot be safely repaired with minimally invasive surgical techniques and will require open surgery.
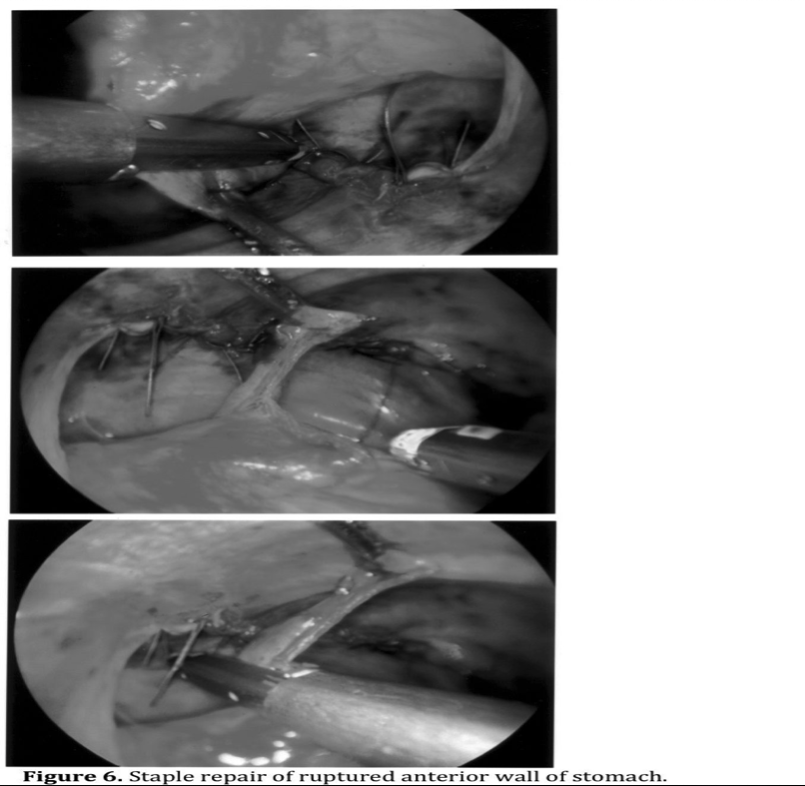
Hollow viscus injuries can be repaired with minimally invasive surgery. Penetrating injury to the anterior wall of the stomach lends itself to repair by intracorporeal suture or stapling (Figures 5 and 6).17,35 A posterior wall perforation can be difficult to identify and requires thorough examination through the lesser sac. Open laparotomy should be performed if a suspected posterior wall injury cannot be identified laparoscopically.
Suture of small bowel perforations can also be repaired with minimally invasive techniques.8,49 Perforations on the mesenteric border may be difficult to visualize. Limited resections can be safely done with intracorporeal suturing or stapling, and mini- laparotomy may be performed to resect bowel and suture extracaporally.8 The same is true for colon injuries for repair, resection with anastomosis, or colostomy.8 The added risk exists of missing a retroperitoneal colon injury. The left or right colon should be mobilized from its retroperitoneal attachments when necessary to examine this area.
Mobilization of the colon may be facilitated by hand-assisted laparoscopic techniques.

Retroperitoneal injuries are often difficult to diagnose by laparoscopic surgery with as many as 60% of retroperitoneal organ injuries reportedly missed.20,22,23 Pancreatic injuries, particularly of the body and tail can be visualized with a laparoscope, and injuries can be drained that do not appear to involve the pancreatic duct. The pancreatic duct can be visualized and evaluated with laparoscopic ultrasound when available.
Reports exist of successful distal pancreatectomy with minimally invasive surgical techniques.3,33
Although laparoscopy has been used extensively in elective renal surgery, little experience has been reported for traumatic injuries to the kidney and other retroperitoneal urological structures. The dome of the bladder is the only portion of the urinary system accessible to laparoscopic repair or definitive diagnosis.
CONCLUSION
The most established role for laparoscopy in trauma is for the diagnosis of abdominal injuries. It may be the best diagnostic test available to assess peritoneal penetration from questionable knife or gunshot wounds. Laparoscopy is the most reliable diagnostic technique to identify, and in many cases repair, diaphragmatic injuries. Specific injuries to solid organs and viscera can be accurately identified to determine the need of actual repair. Laparoscopic screening and diagnosis allows for more accurate use of open laparotomy when significant injuries are identified, thus avoiding the morbidity associated with nontherapeutic laparotomy. Therapeutic applications continue to be limited to repair of minor injuries to the visceral structures and solid organs. Watch for the emergence of SIL into the management of trauma patients. It is not only more cosmetic, but more importantly may have the advantage of better access to all areas of the abdominal compartment over standard laparoscopic techniques. Complex injuries occasionally may be undertaken in the stable patient with the application of hand-assisted laparoscopy, minilaparotomy, or angiographicembolization.
It is important to emphasize the unpredictable and potentially unstable nature of traumatic injuries. The surgeon must always be prepared to rapidly open the abdomen to gain control of hemorrhage. The patient should always be in a supine position, and all instruments needed for an open laparotomy should be in the room and open, available for immediate use.
References
- Short AR. The uses of coelioscopy. BMJ. 1925;2:254-255.
- Stone WE. Intra-abdominal examination by the aid of the peritoneoscope. J Kansas Med Soc. 1924;24:63-65.
- Villavicencio RT, Aucar JA. Analysis of laparoscopy in trauma. J Am Coll Surg. 1999;189:11-20.
- Josephs LG, Este-McDonald JR, Birkett DH, Hirsh EF. Diagnostic laparoscopy increases intracranial pressure. J Trauma. 1994;36(6):815-819.
- Rosenthal RJ, Hiatt JR, Phillips EH, Hewitt W, Demitriou AA, Grode M. Intracranial pressure effects of pneumoperitoneum in a large-animal model. Surg Endosc. 1997;11:376-380.
- Mobbs RJ, Yang MO. The dangers of diagnostic laparoscopy in the head injured patient. J Clin Neuroscience. 2002;9:592-59
- Smith RS, Fry WR. Alternative techniques in laparoscopy for trauma. Trauma Q. 1993;10:291-300.
- Choi YB, Lim KS. Therapeutic laparoscopy for abdominal trauma. Surg Endosc. 2003;17:421-427.
- Feliciano DV. Diagnostic modalities in abdominal trauma. Peritoneal lavage, ultrasonography, computed tomography scanning and arteriography. Surg Clin North Am. 1991;71:241-256.
- Root HD, Hauser CW, McKinley CR, Lafave JW, Mindiola RP Jr. Diagnostic peritoneal lavage. Surgery. 1965;57:633-637.
- Nagy KK, Krosner SM, Joseph KT, Roberts RR, Smith RF, Barrett J. A method of determining peritoneal penetration in gunshot wounds to the abdomen. J Trauma. 1997;43:242-246.
- Merlotti GJ, Dillon BC, Lange DA, Robin AP, Barrett JA. Peritoneal lavage in penetrating thoracoabdominal trauma. J Trauma. 1988;28:17-23.
- Cuschieri A, Hennessy TP, Stephens RB, Berci G. Diagnosis of significant abdominal trauma after road traffic accidents: preliminary results of a multicentre clinical trial comparing minilaparoscopy with peritoneal lavage. Ann R Coll Surg Engl. 1988;70(3):153-155.
- Marx JA, Moore EE, Jorden RC, Eule J Jr. Limitation of computed tomography in the evaluation of acute abdominal trauma: a prospective comparison with diagnostic peritoneal lavage. J Trauma. 1985;25:933-937.
- Sherck JP, Oaks DD. Intestinal injuries missed by computed tomography. J Trauma. 1990;30:1-7.
- Gazzaniga AB, Stanton WW, Bartlett RH. Laparoscopy in the diagnosis of blunt and penetrating injuries to the abdomen. Am J Surg. 1976;131:315-318.
- Zantut LF, Ivatury RR, Smith RS, et al. Diagnostic and therapeutic laparoscopy for penetrating abdominal trauma-a multicenter experience. J Trauma. 1997;42:825-829.
- Salvino CK, Esposito TJ, Marshall WJ, Dries DJ, Morris RC, Gamelli RL. The role of diagnostic laparoscopy in the management of trauma patients: a preliminary assessment. J Trauma. 1993;34:506-515.
- Wood D, Berci G, Morgenstern L, Paz-Partlow M. Mini-laparoscopy in blunt abdominal trauma. Surg Endosc. 1988;2:184-189.
- Rossi P, Mullins D, Thal E. Role of laparoscopy in the evaluation of abdominal trauma. Am J Surg. 1993;166:707-711.
- Mazuski JE, Shapiro MJ, Kaminski DL, et al. Diagnostic laparoscopy for evaluation of penetrating abdominal trauma [abstract]. J Trauma. 1997;42:163.
- Brandt CP, Priebe PP, Jacobs DG. Potential of laparoscopy to reduce nontherapeutic trauma laparotomies. Am Surg. 1994;60:416-420.
- Ortega AE, Tang E, Froes ET, Asensio JA, Katkhouda N, Demetriades D. Laparoscopic evaluation of penetrating thoracoabdominal traumatic injuries. Surg Endosc. 1996;10:19-21.
- Ross SE, Dragon GM, O’Malley KF, Rehm CG. Morbidity of negative celiotomy in trauma. Injury. 1995;26:393-394.
- Renz BM, Feliciano DV. The length of hospital stay after an unnecessary laparotomy for trauma: a prospective study. J Trauma. 1996;40:187-190.
- Weigelt GA, Kingman RG. Complications of negative laparotomy for trauma. Am J Surg. 1988;156:544-547.
- Ditmars ML, Nongard F. Laparoscopy for triage of penetrating trauma: the decision to explore. J Laparoendosc Surg. 1996;6:285-291.
- Cherry RA, Eachempati SR, Hydo LJ, Barie PS. The role of laparoscopy in penetrating abdominal stab wounds. Surg Laparosc Endosc Percutan Tech. 2005,15:14- 17.
- Ivatury RR, Simon RJ, Weksler B, Bayard V, Stahl WM. Laparoscopy in the evaluation of the intrathoracic abdomen after penetrating injury. J Trauma. 1992;33:101- 108.
- Ivantury RR, Simon RJ, Stahl WM. A critical evaluation of laparoscopy in penetrating abdominal trauma. J Trauma. 34: 822-828.
- Matthews BD, Bui H, Harold KL, et al. Laparoscopic repair of traumatic diaphragmatic injuries. Surg Endosc. 2003;17:254-258.
- De Wilt JHW, Van Eijck CHJ, Hussain SM, Bonjer HJ. Laparoscopic spleen preserving distal pancreatectomy after blunt abdominal trauma. Injury Int J Care Injured. 2003;34:233-234.
- Reiff DA, McGwin Jr G, Metzger J, Windham ST, Doss M, Rue LW Identifying injuries and motor vehicle collision characteristics that together are suggestive of diaphragmatic rupture. J Trauma. 2002;53(6):1139-1144.
- Degiannis E, Levy R, Sofianos C, Potokar T, Florizoone MG, Saadia R. Diaphragmatic herniation after penetrating trauma. Br J Surg. 1996;83:88-91.
- Smith RS, Fry WR, Morabito DJ, et al. Therapeutic laparoscopy in trauma. Am J Surg. 1995;170:632-637.
- Bautz P. Laparoscopy in trauma. Trauma Yearbook (1994). Johannesburg: Helm Publishing; 1994:18-20.
- Asbun HJ, Bowyer MW, et al. Hand-assisted laparoscopic exploration for trauma: a false sense of security. Surg Endosc. 2002;12:614.
- Navarra G, Pozza E, Occhinonorelli S, et al. On-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695.
- Vidal O, Valentini M, Ginesta C, et al. Laparoendoscopic single-site surgery appendectomy. Surg Endosc. 2009; Aug 19.
- Jeong BC, Park YH, Han DH, Kim HH. Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol. 2009;23:1957-1960.
- Nguyen NT, Slone J, Reavis K. Comparison study of conventional laparoscopic gastric banding versus laparoendoscopic single site gastric banding. Surg Obes Relat Dis. 2009; Nov 10.
- Canes D, Berger A, Aron M, et al. Laparo-endoscopic single site (LESS) versus standard laparoscopic left donor nephrectomy: matched-pair comparison. Eur Urol. 9009; Jul 28.
- Choi SI, Lee KY, Park SJ, Lee SH. Single port laparoscopic hemicolectomy with D3 dissection for advanced colon cancer. World Journal of Gastroenterology. 2010:16(2):275-278.
- Kaouk JH, Goel RK, Haber GP, Crouzet S, Desai MM, Gil IS. Single port laparoscopic radical prostatectomy. Urology. 2008:72(6):1190-1193.
- Kalimi R, Gorecki PJ, Angus LD, Shaftan GW. Laparoscopic exploration for pancreatic injury. Surg Endosc. 2002;16:217.
- Fabian TC, Croce MA, Stewart RM, Pritchard FE, Minard G, Kudsk KA. A prospective analysis of diagnostic laparoscopy in trauma. Ann Surg. 1993;217:557-565.
- Terrell TR, Lundquist B. Management of splenic rupture and return-to-play decisions in a college football player. Clin J Sport Med. 2000;12(6):00-402.
- Kohler R, Millin R, et al. Laparoscopic treatment of an isolated gallbladder rupture following blunt abdominal trauma in a schoolboy rugby player. Br J Sports Med. 2002;36:378-379.
- Velez SE, Llaryora RG, Lerda FA. Laparoscopic cholecystectomy in penetrating trauma. J Laparoend Adv Surg Tech. 1999;9(3):291-293.
Figures 1-4 courtesy of Michael S. Kavic, MD, FACS.
