Intraperitoneal and Retroperitoneal Anatomy
Douglas Brown, MD, Shaghayegh DeNoble, MD, Ceana Nezhat, MD, Camran Nezhat, MD, and Farr Nezhat, MD
Sound surgical technique, whether during laparotomy or laparoscopy, is based on accurate anatomic knowledge. Laparoscopic surgeons must adapt to the altered appearance of anatomy due to the effects of pneumoperitoneum, Trendelenburg positioning, and traction from a uterine manipulator. There are inherent limitations of laparoscopy related to the fixed visual axis, loss of depth of field, and magnification. Furthermore, laparoscopes with different angles of view make orientation more challenging.
Because a three-dimensional field is projected to video monitors as a two-dimensional image, it is imperative for the endoscopic surgeon to understand that the anatomic structures appearing superior on the monitor are actually anterior and those inferior are posterior.
In this chapter, we describe some important anatomic relations that are critical during laparoscopic procedures.
SUPERFICIAL INTRAPERITONEAL ANATOMY (LANDMARKS TO RETROPERITONEAL STRUCTURES)
Superficial intraperitoneal landmarks within the pelvis alert the operator to key anatomic structures in the retroperitoneal space (Figure 1.1 A-C).
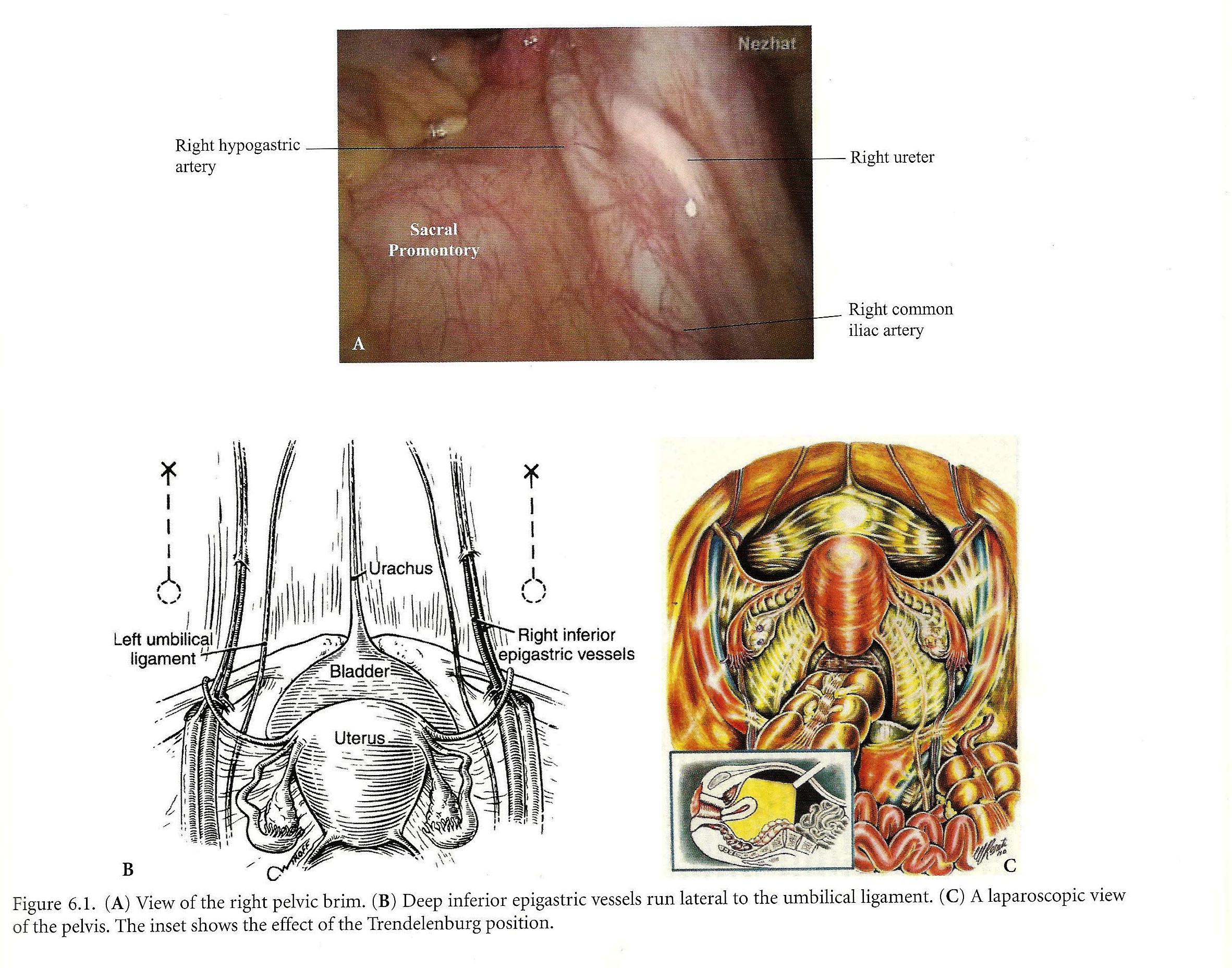 Figure 1.1. (A) View of the right pelvic brim. (B) Deep inferior epigastric vesselsrun lateral to the umbilical ligament. (C) A laparoscopic view of the pelvis.The inset shows the effect of the Trendelenburg position.
Figure 1.1. (A) View of the right pelvic brim. (B) Deep inferior epigastric vesselsrun lateral to the umbilical ligament. (C) A laparoscopic view of the pelvis.The inset shows the effect of the Trendelenburg position.
The umbilicus is located at the level of L3-L4, although the location varies with the patient’s weight, the presence of abdominal panniculus, and the position of the patient on the operating table (supine vs. Trendelenburg). The abdominal aorta bifurcates at L4-L5 in 80% of cases.l
The parietal peritoneum over the anterior abdominal wall is raised at five sites, representing the five umbilical folds. The median umbilical fold, running from the dome of the bladder to the umbilicus, covers the obliterated urachus. Lateral to the urachus, on either side, are the medial umbilical folds, overlying the obliterated umbilical arteries.
Just lateral to each medial umbilical fold is the lateral umbilical ligament (fold), formed by the peritoneum overlying the inferior epigastric vessels before their entry into the rectus sheath as they course cephalad to join the superior epigastric artery. In most cases, their location may be visually confirmed through the laparoscope, avoiding injury to them during the placement of accessory trocars. On either side of the rectouterine pouch, the peritoneum reflects over the uterosacral ligaments, forming the uterosacral folds.
Slightly lateral and superior to the uterosacral fold is often another fold of peritoneum, the ureteric fold, which covers the ureter.
Many additional key structures can be identified transperitoneally before any dissection. The internal iliac artery travels parallel and just posterior to the ureter. The external iliac artery is several centimeters anterior to it on the psoas muscle. The external and internal iliac arteries may then be followed superiorly to find the bifurcation of the common iliac arteries at the pelvic brim overlying the sacroiliac joint. This is an ideal location to identify the ureter traversing the point of bifurcation as it enters the pelvis. The right common iliac artery may then be followed superiorly to the bifurcation of the aorta, above the presacral space at approximately the fourth lumbar vertebra. The left common iliac artery is more difficult to identify because of the overlying mesentery of the sigmoid colon. The left common iliac vein is located just medial and inferior to the left common iliac artery in the presacral space. At times it covers the entire space between the common iliac arteries.
PELVIC BRIM
Multiple important structures enter the pelvic cavity at the pelvic brim and can be appreciated layer by layer (Figure 1.2 A-D). Starting superficially from the peritoneal surface toward the sacroiliac joint, the following structures are found in close proximity to each other and can be recognized laparoscopically as superficial peritoneal landmarks: the peritoneum, the ovarian vessels in the infundibulopelvic ligament, the ureter, the bifurcation of the common iliac artery, and the common iliac vein. Dissecting deeper layers, the medial edge of the psoas muscle, the obturator nerve, and the parietal fascia overlying the capsule of the sacroiliac joint will be exposed. The lumbosacral trunk lies medial to the obturator nerve.
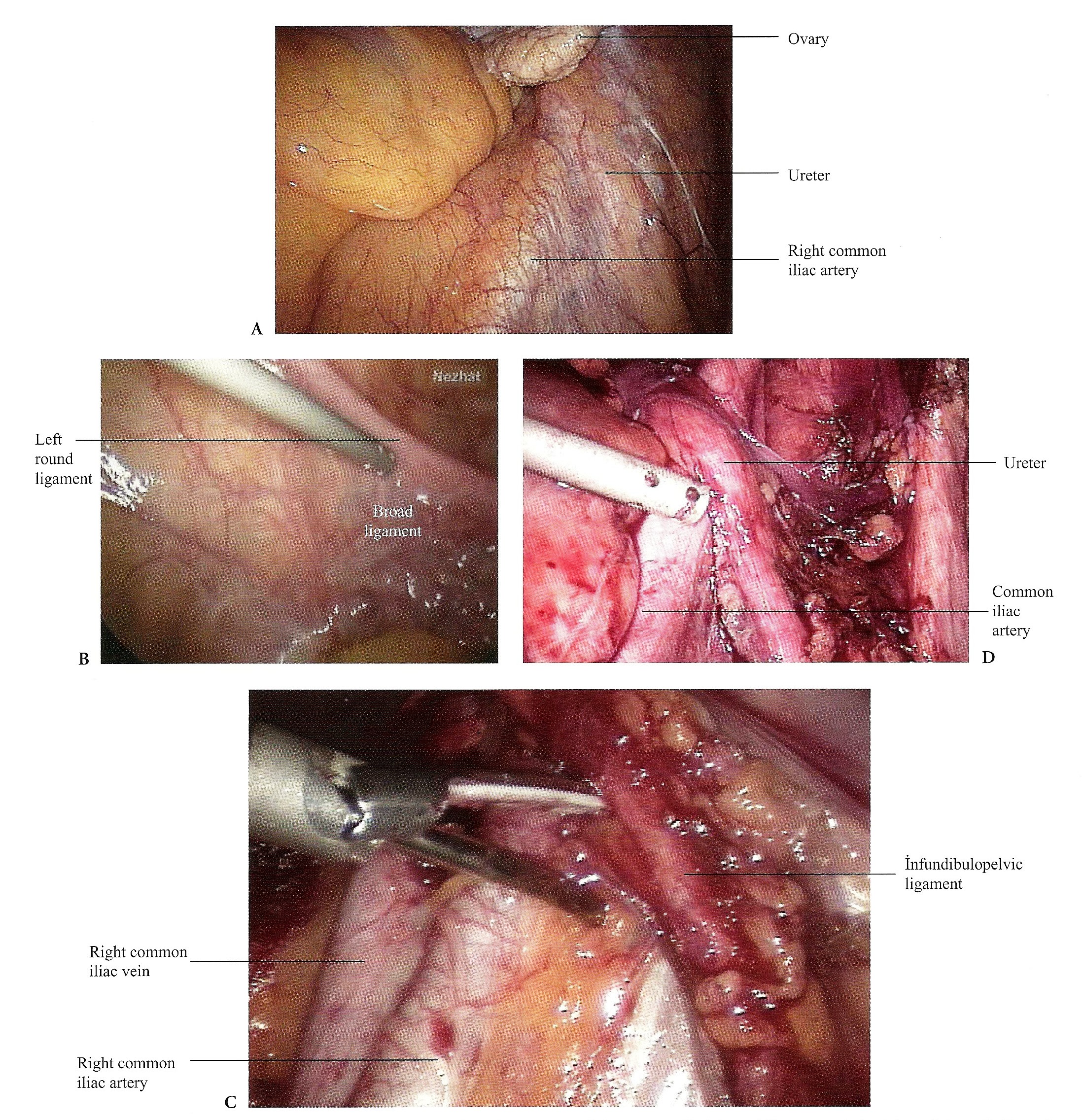 Figure 1.2. (A) The laparoscopic view of the pelvic brim before the incision. (B) A view of left broad ligament. (C) Right pelvic wall dissection during pelvic lymphadenectomy. (D) The dissection of right pelvic sidewall is completed and the crossing of the ureter on common iliac vessels at the pelvic brim is clearly seen.
Figure 1.2. (A) The laparoscopic view of the pelvic brim before the incision. (B) A view of left broad ligament. (C) Right pelvic wall dissection during pelvic lymphadenectomy. (D) The dissection of right pelvic sidewall is completed and the crossing of the ureter on common iliac vessels at the pelvic brim is clearly seen.
PELVIC SIDEWALL
The pelvic sidewall is entered by opening the peritoneal reflection bordered by the round ligament anteriorly, the infundibulopelvic ligament medially, and the external iliac artery laterally (Figures 1.3 A-B, C-D, E-G and 1.4 B). Based on avascular planes, there are three surgical layers.
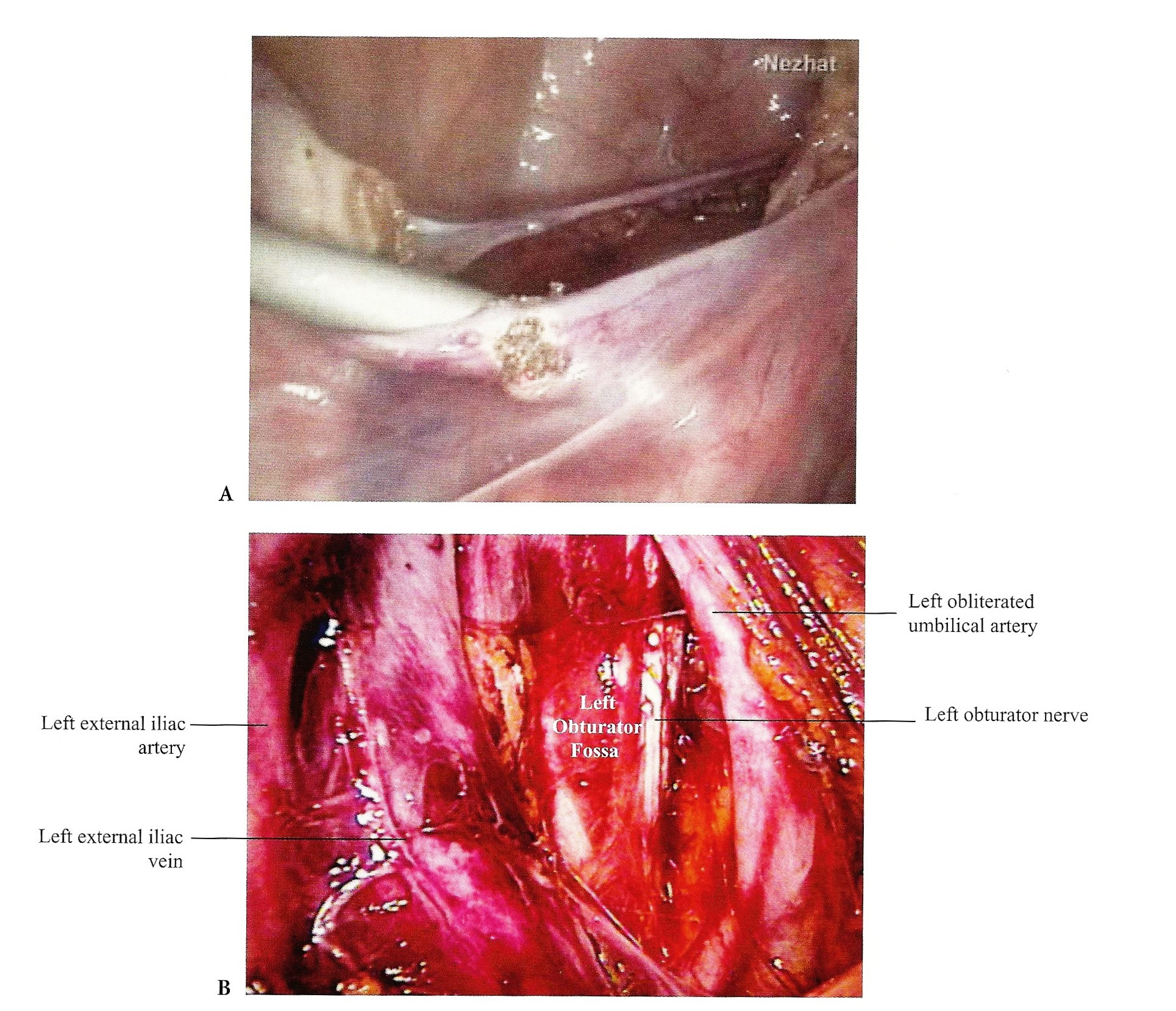 Figure 1.3. (A) An incision is made in the left broad ligament lateral or parallel to the infundibulopelvic ligament to develop the paravesical space. The round ligament can be divide either before or after this space is developed. This incision can be made by the scissors, the harmonic shear, or the CO2 laser. (B) A view of the left obturator fossa.
Figure 1.3. (A) An incision is made in the left broad ligament lateral or parallel to the infundibulopelvic ligament to develop the paravesical space. The round ligament can be divide either before or after this space is developed. This incision can be made by the scissors, the harmonic shear, or the CO2 laser. (B) A view of the left obturator fossa.
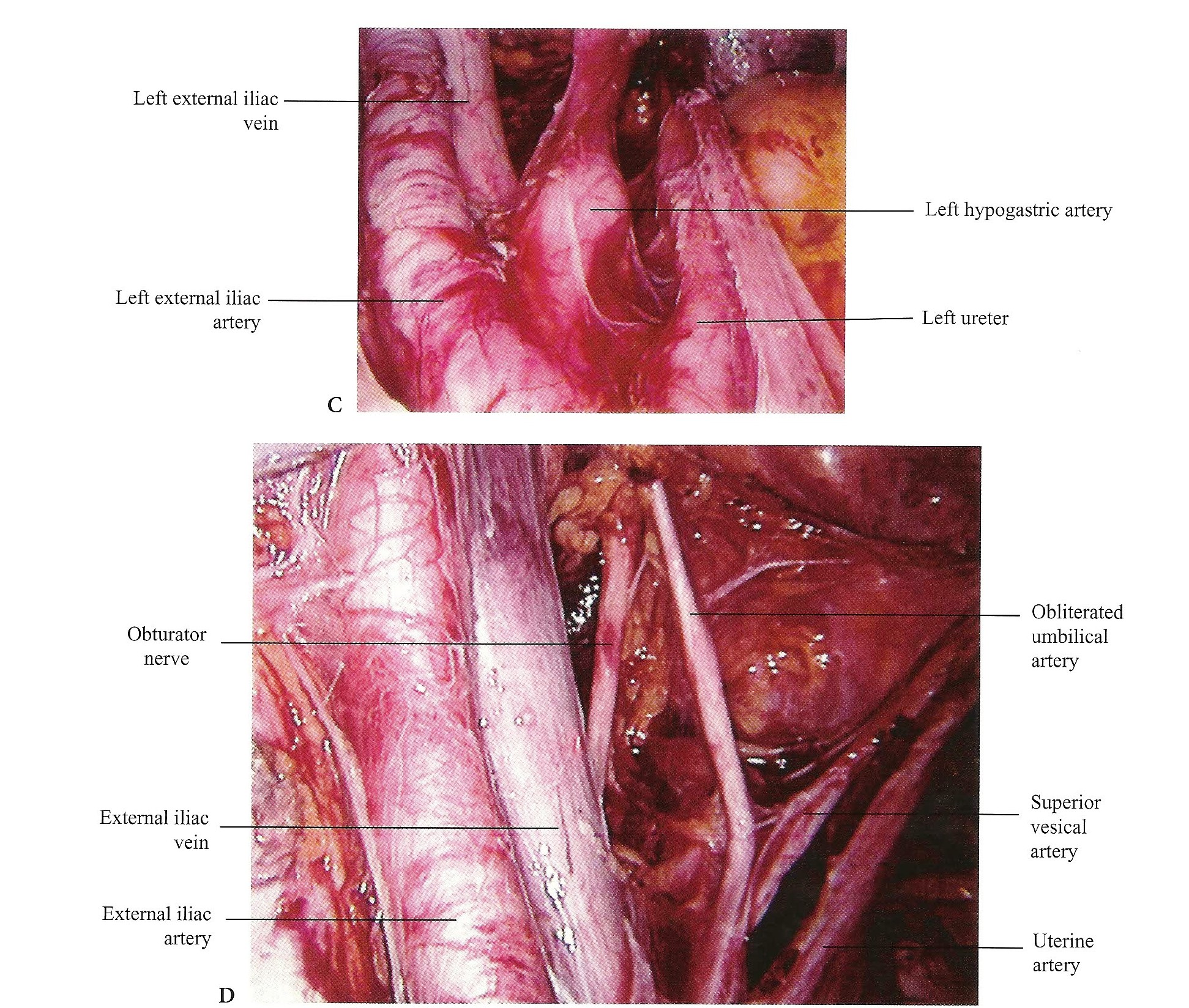 Figure 1.3. (C) An anatomical view of the left pelvic brim. (D) Left pelvic sidewallretroperitoneal anatomy.
Figure 1.3. (C) An anatomical view of the left pelvic brim. (D) Left pelvic sidewallretroperitoneal anatomy.
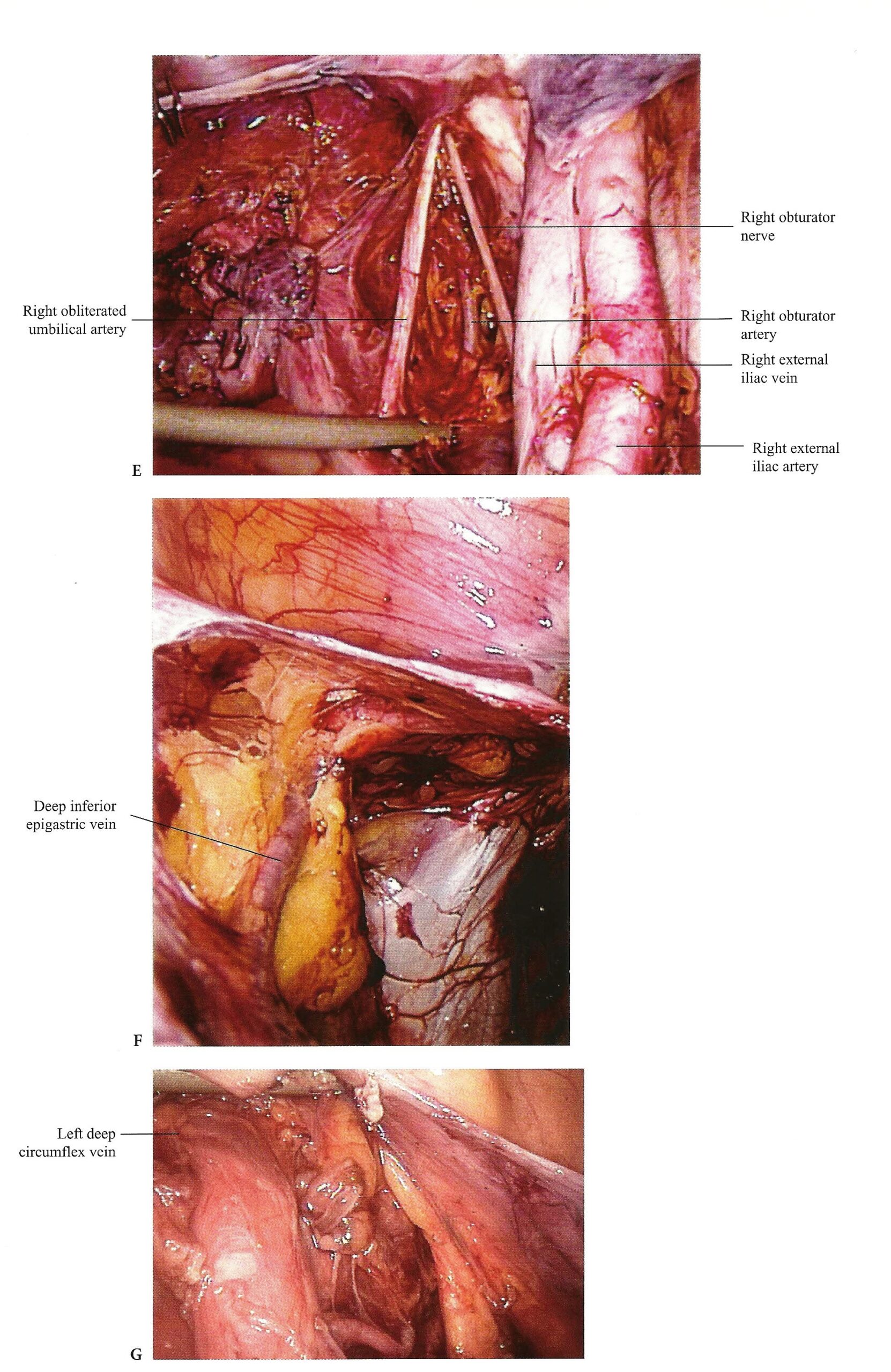 Figure 1.3. (E) Right pelvic sidewall retroperitoneal anatomy. (F) The course of deep inferior epigastric vein from its origin. (G) The deep circumflex vein is identified during pelvic lymphadenectomy.
Figure 1.3. (E) Right pelvic sidewall retroperitoneal anatomy. (F) The course of deep inferior epigastric vein from its origin. (G) The deep circumflex vein is identified during pelvic lymphadenectomy.
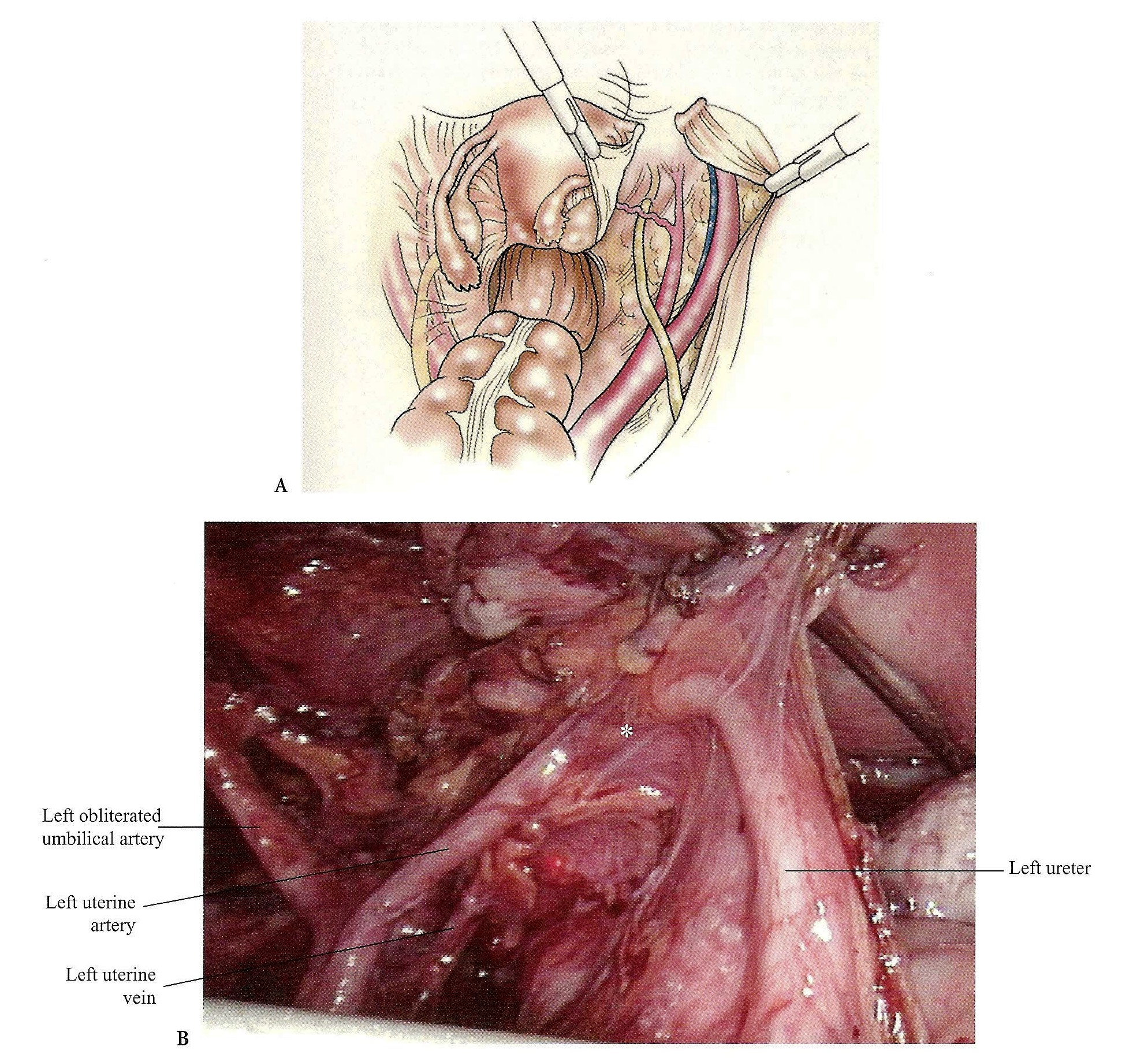 Figure 1.4. (A) Right pelvic side-wall exposure. (B) To prevent injuries, the ureter must be identified before irreversible action is taken. Here is one of the most vulnerable sites of ureteral injury and the anatomy of water under the bridge is clearly seen.
Figure 1.4. (A) Right pelvic side-wall exposure. (B) To prevent injuries, the ureter must be identified before irreversible action is taken. Here is one of the most vulnerable sites of ureteral injury and the anatomy of water under the bridge is clearly seen.
First Layer of the Pelvic Sidewall
Medially, the first layer is the parietal peritoneum with the ureter attached to it in its own fascial sheath. The ureter can be retracted medially by incising this peritoneum, or it can be separated by blunt or hydrodissection.
Second Layer of the Pelvic Side Wall
The second surgical layer consists of the internal iliac vessels and their visceral anterior branches: uterine, superior vesical leading to the obliterated umbilical, inferior vesical, vaginal, and the middle rectal arteries.
Third Layer of the Pelvic Side Wall
From anterior to posterior lie the (i) psoas muscle with the external iliac artery on its medial aspect, (ii) external iliac vein just medial and posterior to it, and (iii) external iliac vein beneath the obturator internus muscle with the obturator nerve and vessels coursing along its anterior border toward the obturator canal.
PELVIC LYMPH NODES
The external pelvic nodes are found along the external iliac artery and vein from the bifurcation of the common iliac vessels to the deep circumflex iliac veins caudally. The obturator nodes are found in the obturator fossa, which is bordered medially by the hypogastric artery; laterally by the external iliac vein, the obturator internus muscle, and its fascia; and anteriorly by the obturator nerve and vessels. The nodes along the hypogastric vessels up to the bifurcation of the common iliac artery and vein comprise the hypogastric group.
BASE OF THE BROAD LIGAMENT
The base of the broad ligament (Figure 1.4 A, B) comprises the cardinal ligament, also known as the ligament of Mackenrodt. Dissection of the pelvic sidewall will lead into this region. It is important to comprehend that the internal iliac artery continues into the superior vesical artery and then into the obliterated umbilical artery. Traction on the medial umbilical fold will help identify the internal iliac artery, and the medial branch passing superior to the ureter can then be identified as the uterine artery. The upper portion of the cardinal ligament is penetrated by the ureter as it travels into the tunnel of Wertheim just beneath the uterine artery, 1 to 2 crn lateral to the isthmus of the uterus, immediately lateral to the uterosacral ligament. This is one of the most common sites of ureteric injury in gynecologic procedures.
The base of the broad ligaments delineates two important spaces: Anteriorly is the paravesical space and just posterior, toward the sacrum, is the pararectal space. The extent of lateral dissection toward the pelvic sidewall and consequently excision of the ligament of Mackenrodt determines the class of radical hysterectomy.
AVASCULAR SPACES OF THE PELVIS
Three pairs of ligaments divide the pelvis into eight avascular spaces (Figure 1.5 A, B).
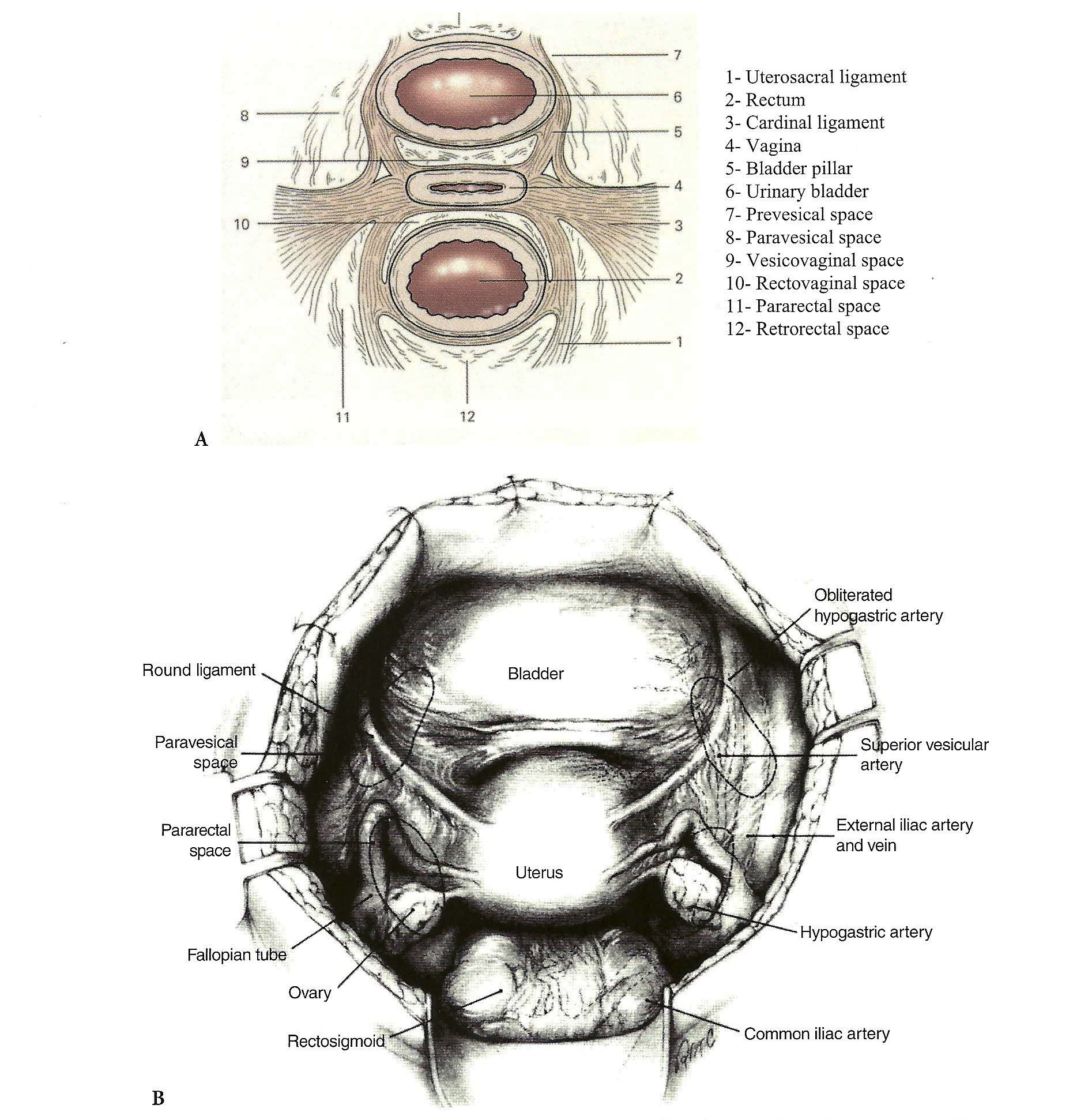 Figure 1.5. (A) Avascular spaces and their ligamental boundries. (B) Illustrated are the eight avascular spaces and their anatomic relationship during the laparatomy.
Figure 1.5. (A) Avascular spaces and their ligamental boundries. (B) Illustrated are the eight avascular spaces and their anatomic relationship during the laparatomy.
Prevesical (Retropubic) Space of Retzius
The space of Retzius, or the retropubic space, is a potential avascular space with vascular borders between the back of the pubic bone and the anterior wall of the bladder (Figure 1.6).
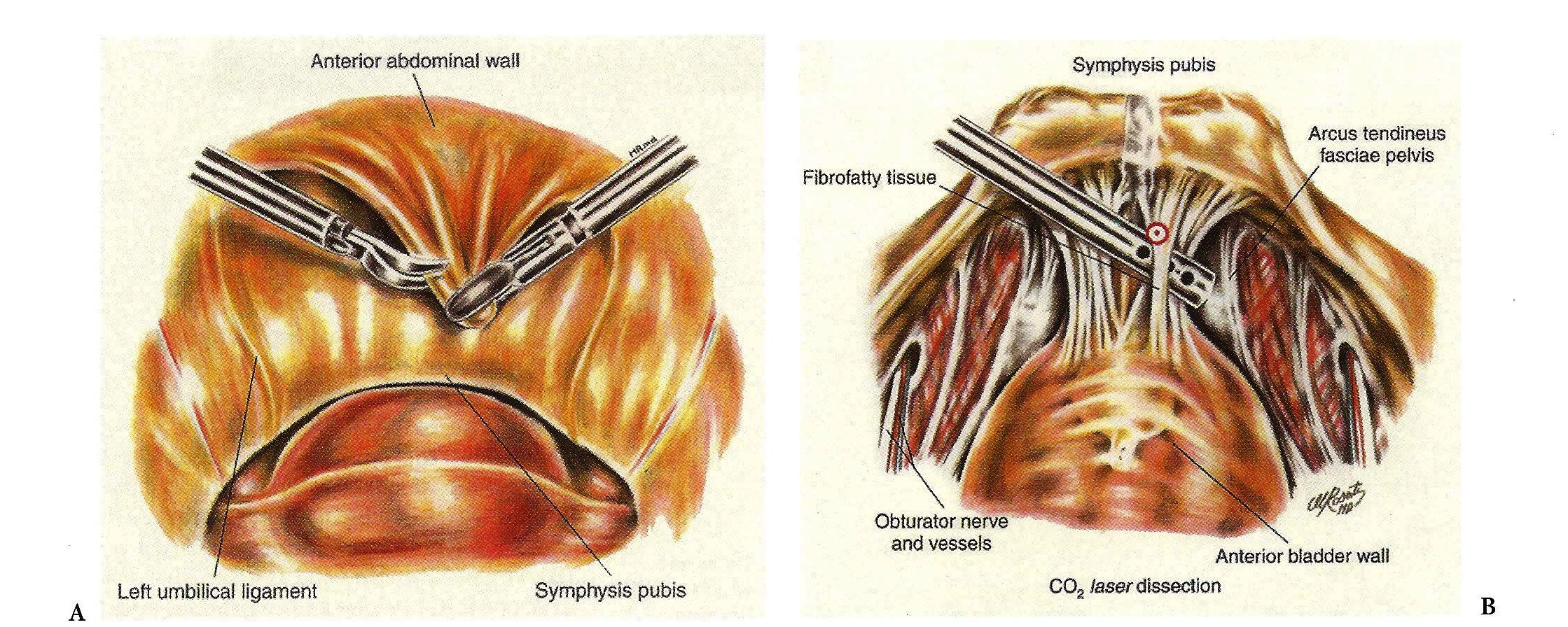 Figure 1.6. (A) A posterior view of the anterior abdominal wall during the Retzius space development (B) The space of Retzius is developed with blunt and sharp dissection of fibrofatty tissue. Care is taken to avoid periurethral neurovascular injury.
Figure 1.6. (A) A posterior view of the anterior abdominal wall during the Retzius space development (B) The space of Retzius is developed with blunt and sharp dissection of fibrofatty tissue. Care is taken to avoid periurethral neurovascular injury.
The retropubic space is bounded anteriorly by the transversalis fascia, which inserts on the posterior surface of the pubic symphysis. The urethra, the paraurethral (pubourethral) ligaments, and the urethrovesical junction (bladder neck) form the floor of this space. The pubic symphysis and the adjacent superior pubic rami with Cooper’s ligament represent the inferior limit.
Paravesical Space
Laterally, the retropubic space is contiguous with the paravesical spaces (Figure 1.7 A, B), their point of separation being the medial umbilical ligaments (obliterated umbilical arteries). The paired paravesical space is bound laterally by the obturator internus muscle and the obturator nerve, artery, and vein, just beneath the bony arcuate ridge of theileum. The posterior border (toward the sacrum) is the endopelvic fascial sheath around the internal iliac artery and vein and its anterior branches, as they course toward the ischial spine. The pubocervical fascia forms the floor of this lateral compartment as it inserts into the arcus tendineus fasciae pelvis (fascial white line). The muscular white line (arcus tendineus levator ani), which is the origin of the levator ani muscles, is just above the level of the fascial white line. Accessory obturator arteries and veins are often present and course from the inferior epigastric vessels and drape across the pectineal (Cooper’s) ligament on their way to anastomose with the obturator vessels in the obturator canal. The surgeon must always look for them, such as in the case of a retropubic colposuspension, because they are present in approximately 40% of patients.
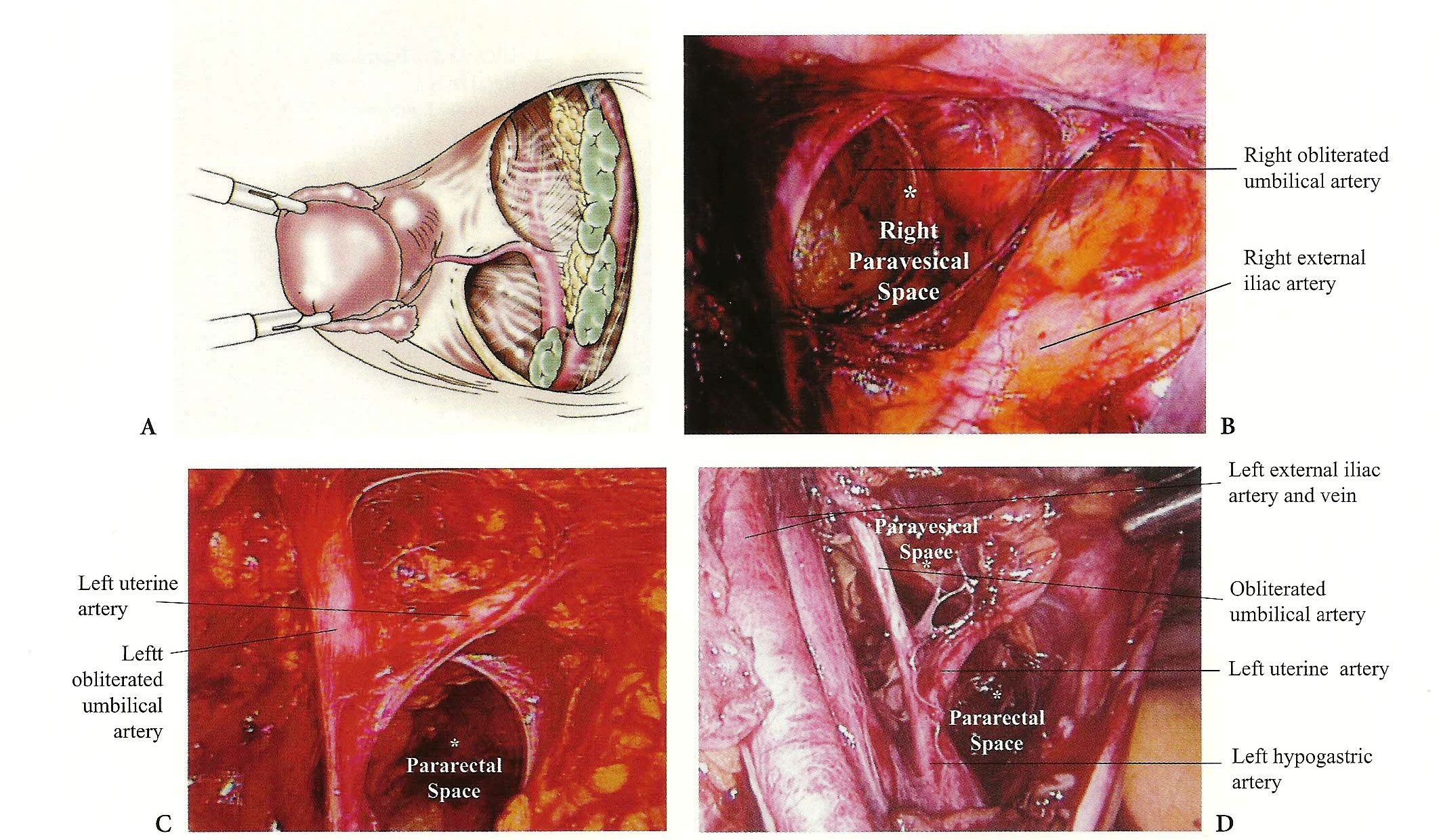 Figure 1.7. (A) The right paravesical space is developed. (B) The paravesical spaces limited by obturator internus muscle and the pelvic diaphragm laterally, the bladder pillar medially, the endopelvic fascia inferiorly, uterine artery posteriorly, and the medial umbilical ligaments superiorly. (C) The pararectal spaces are limited by the levator ani laterally, by the rectal pillars medially, by the anterolateral aspect of sacrum posteriorly, and uterine and cardinal complex anteriorly. (D) The relationship of pararectal and paravaginal spaces with the uterine artery.
Figure 1.7. (A) The right paravesical space is developed. (B) The paravesical spaces limited by obturator internus muscle and the pelvic diaphragm laterally, the bladder pillar medially, the endopelvic fascia inferiorly, uterine artery posteriorly, and the medial umbilical ligaments superiorly. (C) The pararectal spaces are limited by the levator ani laterally, by the rectal pillars medially, by the anterolateral aspect of sacrum posteriorly, and uterine and cardinal complex anteriorly. (D) The relationship of pararectal and paravaginal spaces with the uterine artery.
Pararectal Space
The pararectal space is triangular, with the base of the cardinal ligament representing the anterior border (Figure 1.7 C, D). The medial border is the ureter and the lateral border is the internal iliac artery. This space can be easily developed by bluntly dissecting posterior to the origin of the uterine artery and lateral to the ureter.
Vesicovaginal and Rectovaginal Spaces
The vesicovaginal space is a potential avascular space between the anterior surface of the vagina and the posterior aspect of the bladder, bordered laterally by the bladder pillars or the vesicouterine/vesicocervicalligaments (Figure 1.8 A-C). Entry to this space can be accomplished by incising the vesicouterine fold of peritoneum.
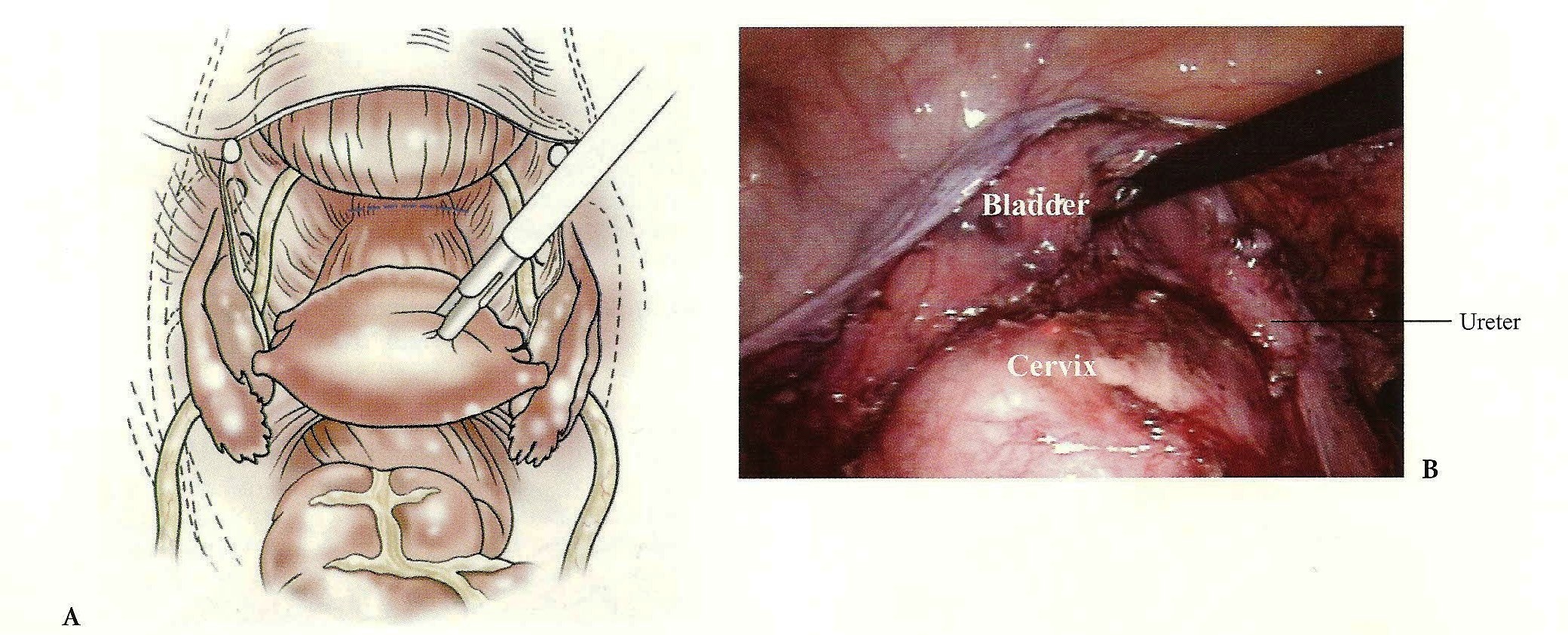
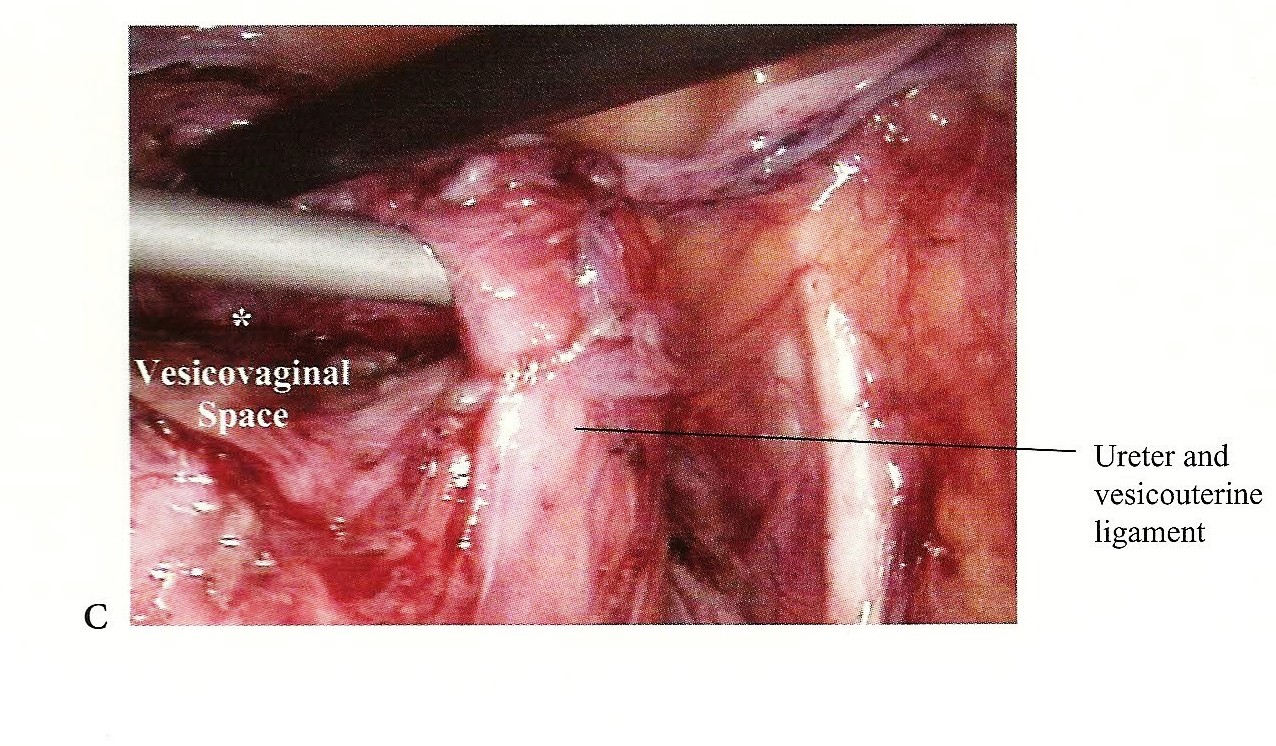 Figure 1.8. (A) The vesicouterine space is a narrow cul-de-sac between the anterior surface of the uterus and the cervix and the upper surface of the bladder when the uterus is in normal anteflexed position. (B) The vesicouterine and vesicovaginal spaces are developed. (C) Precise and continuous attention to the location of the ureter will reduce the incidence of complications.
Figure 1.8. (A) The vesicouterine space is a narrow cul-de-sac between the anterior surface of the uterus and the cervix and the upper surface of the bladder when the uterus is in normal anteflexed position. (B) The vesicouterine and vesicovaginal spaces are developed. (C) Precise and continuous attention to the location of the ureter will reduce the incidence of complications.
The rectovaginal space is bounded by the vagina anteriorly, the rectum posteriorly, and the perineal body inferiorly and laterally (Figure 1.9 A-C). The space is entered by incising the posterior cul-de-sac peritoneum between the two uterosacral ligaments, which lies superiorly.
 Figure 1.9. (A) The rectouterine (rectovaginal) space. The entire space, bounded anteriorly by the cervix and by the fornix in the midline, the uterosacral folds laterally, and the rectum posteriorly. (B) The rectovaginal space is completely developed. (C) Once all ligaments are dissected, all the spaces open to each other.
Figure 1.9. (A) The rectouterine (rectovaginal) space. The entire space, bounded anteriorly by the cervix and by the fornix in the midline, the uterosacral folds laterally, and the rectum posteriorly. (B) The rectovaginal space is completely developed. (C) Once all ligaments are dissected, all the spaces open to each other.
Presacral (Retro-rectal) Space
The retro-rectal space is between the rectum anteriorly and the sacrum posteriorly (Figure 1.10). This space is entered abdominally by dividing the mesentery of sigmoid colon or through the pararectal spaces. Inferiorly this space terminates at the level of the levator muscle and laterally continues as the pararectal fossae. The middle sacral artery and a plexus of veins are attached superficial to the anterior longitudinal ligament of the sacrum. The endopelvic fascia in this space envelops the visceral nerves of the superior hypogastric plexus and the lymphatic tissue. The lateral boundary of the presacral space is formed by the common iliac artery, ureter, and inferior mesenteric artery traversing through the mesentery of the sigmoid colon on the left side.
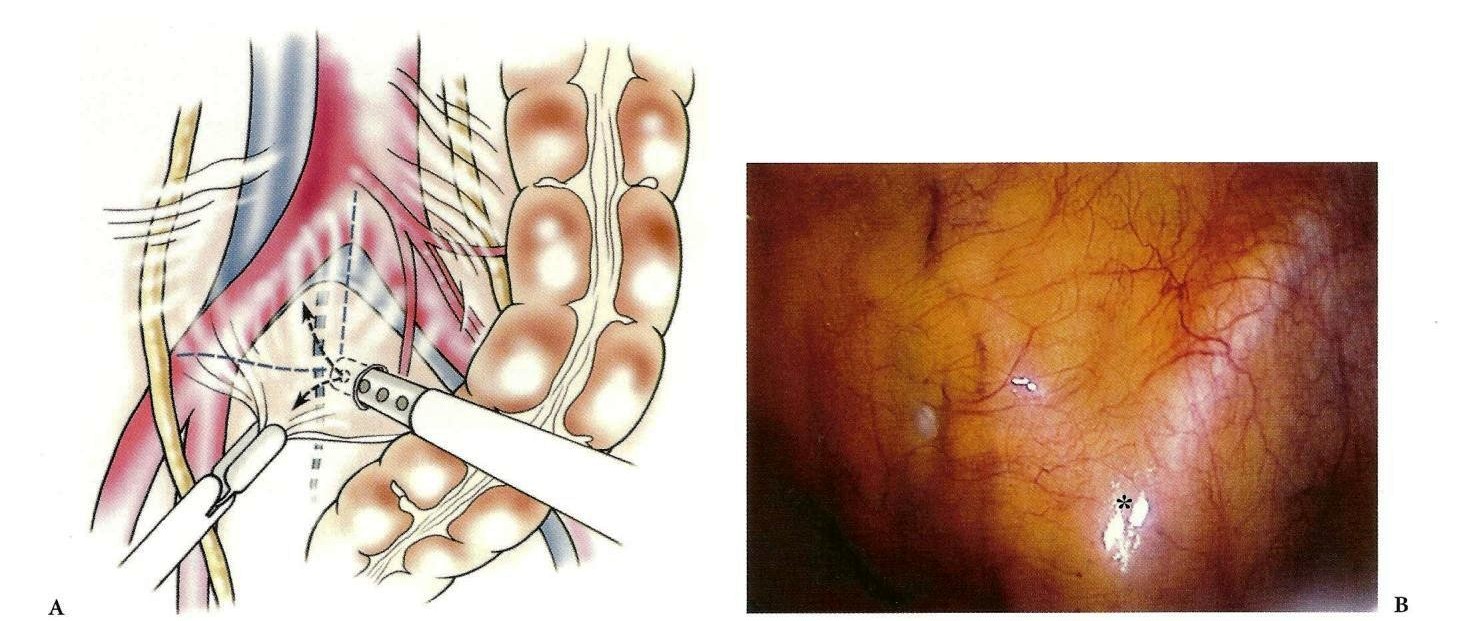
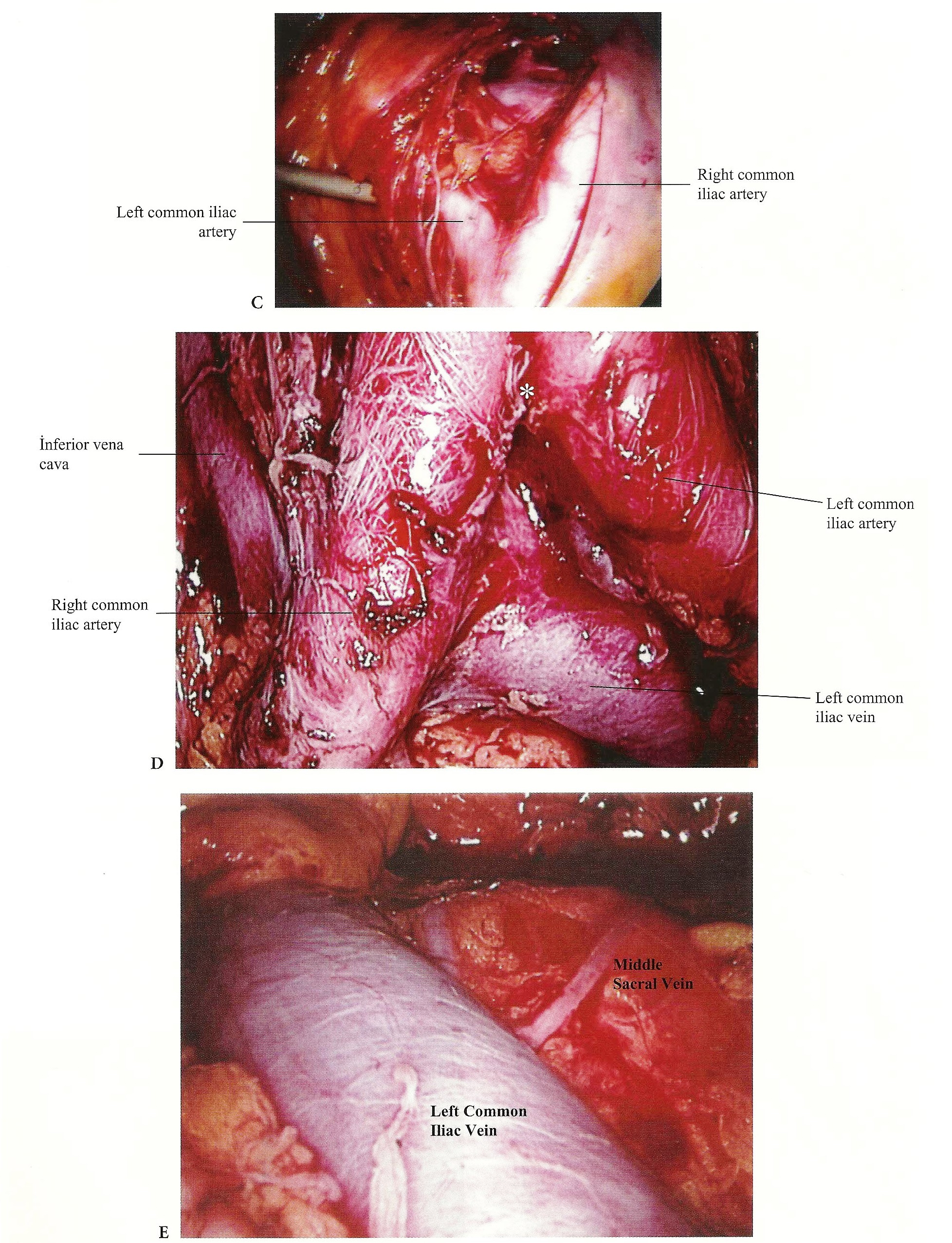 Figure 1.10. (A) Exposure of aortic caval bifurcation. (B) Intraperitoneal view of the bifurcation of the aorta (*). (C) Retroperitoneal view of the bifurcation of the aorta. (D) Anatomic relationships of the bifurcation of the aorta and inferior vena cava. (E) The middle sacral vessels are in the midline on the sacrum. Care must be taken during dissection of this region.
Figure 1.10. (A) Exposure of aortic caval bifurcation. (B) Intraperitoneal view of the bifurcation of the aorta (*). (C) Retroperitoneal view of the bifurcation of the aorta. (D) Anatomic relationships of the bifurcation of the aorta and inferior vena cava. (E) The middle sacral vessels are in the midline on the sacrum. Care must be taken during dissection of this region.
Lateral and inferior dissection in the presacral space leads to the structures entering the pelvis over the pelvic brim.
THE PARA-AORTIC REGION
The para-aortic region is the anatomic area from the renal vessels down to the bifurcation of the common iliac arteries in the posterior abdominal retroperitoneum (Figure 1.11 A- E). For practical purposes, this region is divided into two areas.
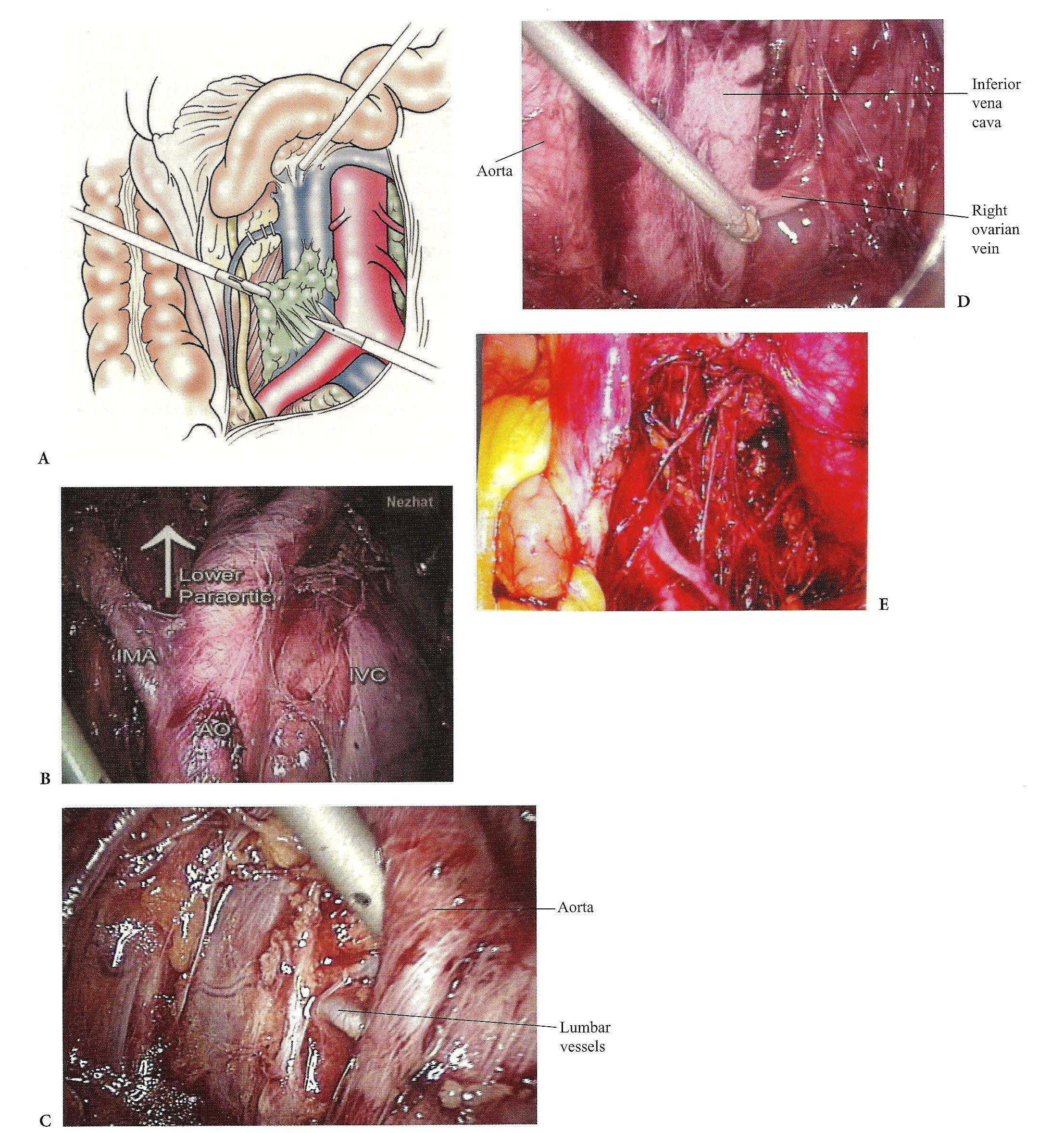 Figure 1.11. (A) The lymph nodes along the right side of the aorta are removed. (B) An anatomical view of the inferior mesenteric artery (IMA) and its origin from the aorta. (C) Anatomic relationships of the lumbar vessels to the aorta. (D) Anatomic relationships of the drainage of the right gonadal vein to LV.C. (E) Anatomic view of the left upper para- aortic area after the lymphadenectomy.
Figure 1.11. (A) The lymph nodes along the right side of the aorta are removed. (B) An anatomical view of the inferior mesenteric artery (IMA) and its origin from the aorta. (C) Anatomic relationships of the lumbar vessels to the aorta. (D) Anatomic relationships of the drainage of the right gonadal vein to LV.C. (E) Anatomic view of the left upper para- aortic area after the lymphadenectomy.
The lower para-aortic area is bounded by the bifurcation of the aorta up to the level of the inferior mesenteric artery superiorly, the psoas muscles laterally, and the bifurcation of the common iliacs inferiorly. Dissections for lymphatic tissue for uterine or cervical cancer involve this area.
The infrarenal area (upper para-aortic area) extends from the level of the inferior mesenteric artery up to the left renal vein. Usually the ovarian arteries exit the anterior aspect of the aorta in the midportion of this area. The right ovarian vein travels next to the right ureter and empties into the vena cava. The left ovarian vein travels with the left ureter but empties into the left renal vein. These structures lie on the anterior surface of the psoas muscle. A major concern on the left side is injury to the renal vein and the lumbar veins and arteries arising from the posterior aspect of the aorta and vena cava.
The inferior extension of this region is the “presacral” space.
The landmarks, which should be kept in mind for para -aortic lymphadenectomies, from right to left are the psoas muscle; ovarian vessels; right ureter, medial to the psoas muscle and lateral to the inferior vena cava; vena cava to the right lateral of the aorta; and aorta and both common iliac arteries. Below the bifurcation of the aorta superficially is the superior hypogastric nerve plexus and the presacral nodes, and beneath them, the left common iliac vein crossing from the left to the right. On the left side of the aorta are the inferior mesenteric artery, the sigmoid colon, and its mesentery. On a deeper plane are the lumbar veins and artery medially and the left ureter laterally, which can be seen after left lymphadenectomy. On the far left is the left psoas muscle (Figure 1.11 C).
THE URETER
The lumbar ureter lies on the psoas muscle medial to the ovarian vessels (Figures 1.2 D, E, 1.4 B, and 1.11 A, B). It enters the pelvic cavity just superficial to the bifurcation of the common iliac artery and just deep to the ovarian vessels, which lie in the infundibulopelvic ligament at the pelvic brim. It lies in the anterior medial leaf of the broad ligament as it courses toward the bladder and can be recognized by its characteristic peristaltic motion. The ureter then passes just lateral to the uterosacral ligament, approximately 2 cm medial to the ischial spine through the upper part of the cardinal ligament at the base of the broad ligament. Here it lies justbeneath the uterine artery, approximately 1.5 to 2 ern lateral to the side of the cervix. The ureter forms a “knee” turn at this point and travels medially and anteriorly to pass on the anterolateral aspect of the upper third of the vagina toward the bladder (Figures 1.4 A, B and 1.9 C).
Reference
- Nezhat F, Brill AI, Nezhat CH, et al. Laparoscopic appraisal of the anatomic relationship of the umbilicus to the aortic bifurcation. JAm Assoc Gynecol Laparosc. 1998;5: 135.
Suggested Reading
Morrow CP, Curtin JP. Surgical anatomy. In: Gynaecologic Cancer Surgery. New York: Churchill Livingstone; 1996:67-139.
Nezhat CR, Siegler AM, Nezhat F, Nezhat C, Seidman DS, Luciano A. Operative Gynecologic Laparoscopy. 2nd ed. New York: McGraw.
Hill; 2000. Pasic RP, Levine RL. A Practical Manual of Laparoscopy: A Clinical Cookbook. Lancashire, UK: Parthenon Publishing Group; 2002.
Rogers RM Ir, Childers JM. Laparoscopic Gynecologic Anatomy.The Surgical Essentials.
Smith JR, Del Priore G, Curtin 1,Monaghan JM. An Atlas of Gynecologic Oncology. London: Martin Dunitz; 2001.
