Reduced Port Surgery: Minimizing Minimal Access Surgery
Erica R. Podolsky, MD, Stephanie A. King, MD, Paul G. Curcillo II, MD
HISTORY
Over the last few years, minimally invasive surgery has seen great changes. Innovations to further minimize incisions have created a new focus in the world of laparoscopy. The introduction of NOTES inspired the concept of incisionless surgery. Just as with the introduction of multiport laparoscopy in the late 1980s and early 1990s, again we see the possibility of improved surgical outcomes in terms of pain, recovery, and need for full sterilization compared with traditional multiport laparoscopy.1
However, as with many new procedures, new approaches come with increased demand on technical skills, a need for training techniques, as well as the potential for new possible complications and adverse outcomes. Although the latter will often slow down adoption of new techniques, if less technical ability is necessary, we may frequently see an increased adoption ahead of proven benefits and the desired risk/benefit assessment.
Preceding the introduction of NOTES, innovative surgeons reported reduced-port and single-incision procedures.2,3 Either because these novel approaches appeared too early after the initial introduction of laparoscopy or because they failed to show improved outcomes, widespread acceptance was not seen. In addition, the techniques used did require some increased skill levels in a still relatively young field. This novel concept of port reduction was limited to select patients and simple procedures, which may have also contributed to the lack of progression.
Although initially begun in the early 1900s,4 laparoscopy had limited applications and saw a slow adoption rate with a steady course of improvements spanning decades. A dramatic increase in adoption occurred in the late 1980s and early 1990s when laparoscopy was applied to the cholecystectomy. Over the next 20 years, advances in laparoscopy again slowed during a maturation phase. Growth was lateral, with applications to virtually all other procedures, but vertical growth was limited. With the exception of the tissue-sealing devices and trocar development, instrumentation and techniques changed very little.
Over the last 3 years, we have seen the emergence of the desire to further improve on multiport laparoscopy, indicating the landscape may be ready for a change. Fueled by the desire to maximize the benefits of laparoscopy, and perhaps by the appearance of NOTES, port reduction has again moved to the forefront of laparoscopy. Progression to a single incision, often hidden within the umbilicus, has become a reality.
In 2007, single-port access surgery was introduced.5,6 Subsequently, a number of transumbilical techniques and modifications have been developed and reported.7-14 Although initially met with skepticism and criticism, single-port laparoscopy has become a hot topic in minimally invasive surgery. Presently, we are seeing a flurry of case reports and initial procedures being accomplished through a variety of these techniques. Often, we are seeing the introduction of a novel device or instrument with claims of facilitating the procedure. Although successful in the pioneers’ hands, the true success will be in applicability and safe outcomes when applied by large numbers of surgeons to large numbers of patients.
Attention to safety and recognition of basic tenets of safe principles will need to be strongly enforced, or we may see the undesired result of increased complications and poor outcomes, putting patients at risk. Naturally, this could lead to the procedures again being shelved as they almost were in the late 1990s.15-17
In addition, because no randomized studies have yet to be completed comparing reduced port techniques with standard multiport procedures, potential benefits and advantages over multiport have not been proven and as of yet may only be cosmetic. Despite this, acceptance and use of these techniques has been seen internationally. We certainly need to keep this in mind as we move forward.
INDICATIONS
In the current age of minimal access surgery, virtually all procedures performed using the laparoscopic approach have been described. Some are easily performed by the majority of surgeons, with some being reserved to the hands of those more adept in laparoscopy. Although only in its infancy, we are again seeing this trend in reduced-portsurgeries.
Several reports have demonstrated a similar application to various procedures using reduced-port techniques. Some have been reserved to cholecystectomy or oophorectomy,18 while some have seen more challenging applications in urologic19 or colorectal surgery.20 Some platforms, such as single-port access surgery, have been applied across the breadth of general surgery21,22 as well as across subspecialties including gynecology and urology. However, it is clear that results are still early, and both effective applications to more complex procedures as well as outcomes will need to be studied.
In the beginning of laparoscopy, contraindications to performing laparoscopic procedures were extensive. With experience, we saw a slow elimination of some contraindications to the point where we are now with a limited number of contraindications persisting. This same process of selecting patients, and in fact, deselecting patients, should be applied to the reduced-port techniques as well. We need to first become proficient at performing the simple procedures with basic dissection skills prior to advancing to more complex or difficult procedures. Further, unlike taking the large step from open to multiport laparoscopy, reduced-port surgery offers us the opportunity to progress in a step-wise fashion as we become more comfortable performing procedures. Reports have demonstrated that we can do complex and difficult cases, but they should not be the starting point for any surgeon. Initial reports in single-port access were simple G-tube placements,23 appendectomies, and catheter placements. Although application of this approach to the gallbladder and ovary came with time, these common procedures may again be viewed as the primary procedures to learn the basics as a springboard to advancing skills.
The single-port access technique in the next few years may potentially be offered for all procedures to all patients who are candidates for minimally invasive surgery. At this point, we need to be cautious not to move too fast. A selection bias may be advantageous, especially in the early implementation of the technique. Because operative times will most likely be extended in initial cases as with any new procedures, this must be considered. Patients with an ideal body weight without a surgical history are ideal, especially for initial cases.
Although specific populations have not been identified, single-port access may be beneficial when decreasing the number of incisions would be helpful. In patients with an altered wound-healing capability, one incision may be desirable. Patients with ascites may also benefit, because drainage will be contained to a single incision. The obese population, with increasing numbers of elective weight loss procedures, may be ideal.
These indications and contraindications will again need to be evaluated as they were with the advent of multiport laparoscopy on an individual basis.
TECHNICAL CONSIDERATIONS
One of the primary goals of advancing a new platform in minimally invasive surgery should be successful applications with maintenance of safe standards. Standard dissection principles and techniques have been developed as laparoscopy has expanded. As we reduce the number of port sites, it is important to adhere to these principles of exposure and dissection to ensure safe and reproducible outcomes. Although some single-port access techniques utilize standard equipment and operative technique, some reduced-port techniques introduce new variables or approaches. Changing techniques is certainly acceptable, provided basic laparoscopic principles are adhered to safely. Recognizing these changes will ensure safe adoption of the technique.
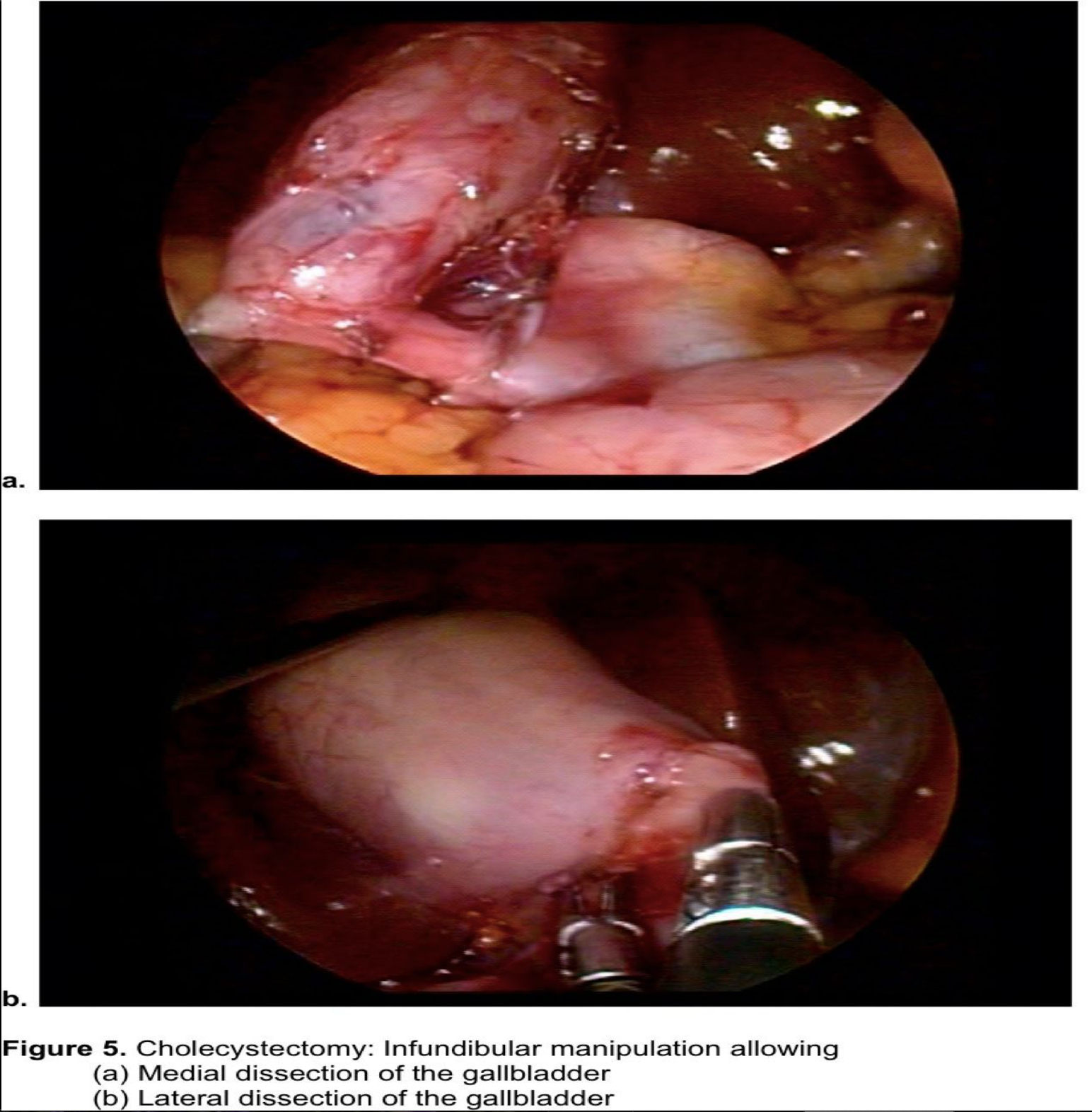
This same transition process was seen with the move from open to laparoscopic procedures. For example, in cholecystectomy, the basic technique of independent fundal retraction and infundibular manipulation with Kelley clamps was maintained with two laparoscopic graspers. In both the open and laparoscopic techniques, the cystic duct is retracted from the common bile duct in an identical fashion ensuring a familiar and safe exposure. The concept of traction and countertraction in colon surgery was also maintained in the transition from open to laparoscopic techniques. Visualization of the ureters during ovarian resections needs to be maintained as well. These mainstays of safety, as well as many others, must be recognized and preserved.
Initial Access
For most reduced-port procedures, a single incision is typically hidden within the umbilicus. Allowing natural skin folds to dictate the orientation of the incision generally results in optimal cosmesis. In some advanced procedures, the umbilicus may not be the best option (ie, ventral hernias and retroperitoneal procedures).
At present, several options are available to the surgeon for the single-port approach. Placement of multiple trocars through separate fascial incisions within the single umbilical incision as described in the single-port access technique has been demonstrated across a large variety of procedures safely over the past 3 years.21 Although cost efficient, placement of the multiple trocars with flaps can be technically challenging at first. Other options include use of multi-trocared single-port devices with multiple lumens, allowing for several instruments and a camera to be passed through one combined skin and fascial incision. Perhaps easier to place, these devices can be costly and have been shown to restrict movement of the individual instruments.24,25
All surgeons should expose themselves to the varying forms of access and choose the one with which they are the most comfortable. A number of properties and characteristics of each platform need to be studied as we cultivate this arena. Currently under investigation are the effects of these techniques on the independence of movement of the individual instruments. The ergonomics in terms of tension against which our hands and forearms are working during dissection and the tension created against the instruments themselves all need to be considered as well. These factors are different with each access device.25
From a patient standpoint, a selection bias for body habitus or BMI may be advantageous. A thinner abdominal wall may enable a wider range of motion and produce less strain on the operator. The ergonomics studies are not yet complete but will determine the comfort level and stress with which we operate in this fashion.
The potential for an increase in access site hernia (ASH) formation also needs to be monitored. We are now introducing a new access technique that is different from standard laparoscopy, and we need to follow this. Although preliminary data demonstrate no increase in hernia formation, it does show loss of the independent movement of instruments when placed though a single-port device.
As with any minimally invasive surgery, an initial look around the abdomen is advantageous. Occasionally, especially in patients who have undergone previous surgery, dense adhesions may preclude the single-port technique or laparoscopy in general. In this situation, a second port site or conversion to open as with multiport laparoscopy is advised.
For the single-port access technique,26 using multiple trocars within one incision, entry into the abdominal cavity remains standard to multiport procedures. A single 5-mm trocar is inserted either by direct visualization or after insufflation by Verress needle. The abdomen is then inspected to decide whether to continue with single-port access, transition to multiport, or to perform an open procedure. After inspection, the abdomen is partially desufflated, allowing creation of skin flaps. Two very low profile 5-mm trocars are then inserted in a triangulated arrangement within the incision. The skin flaps permit space between each trocar, creating a triangulated separation at the abdominal wall. An additional transfascial retractor is often inserted inferiorly within this incision.
The multiport access devices are generally inserted into a single, larger incision made directly through the fascia. The device is then inserted with a Kelly or with the provided introducer.
Visualization
A major difference between multiport and single-port laparoscopy is the orientation of visualization. The midline view with instruments entering from the lateral aspect is replaced with an axial, or in-line view. This needs to be approached cautiously as one “relearns” localization of instruments. There can also be an alteration of depth perception.
Upon inserting subsequent instruments, the operator needs to remember to pull back the camera and localize the incoming instrument to safely insert and follow it into the operative field. Again, as with multiport procedures, with time and experience, this will become easier to accomplish.
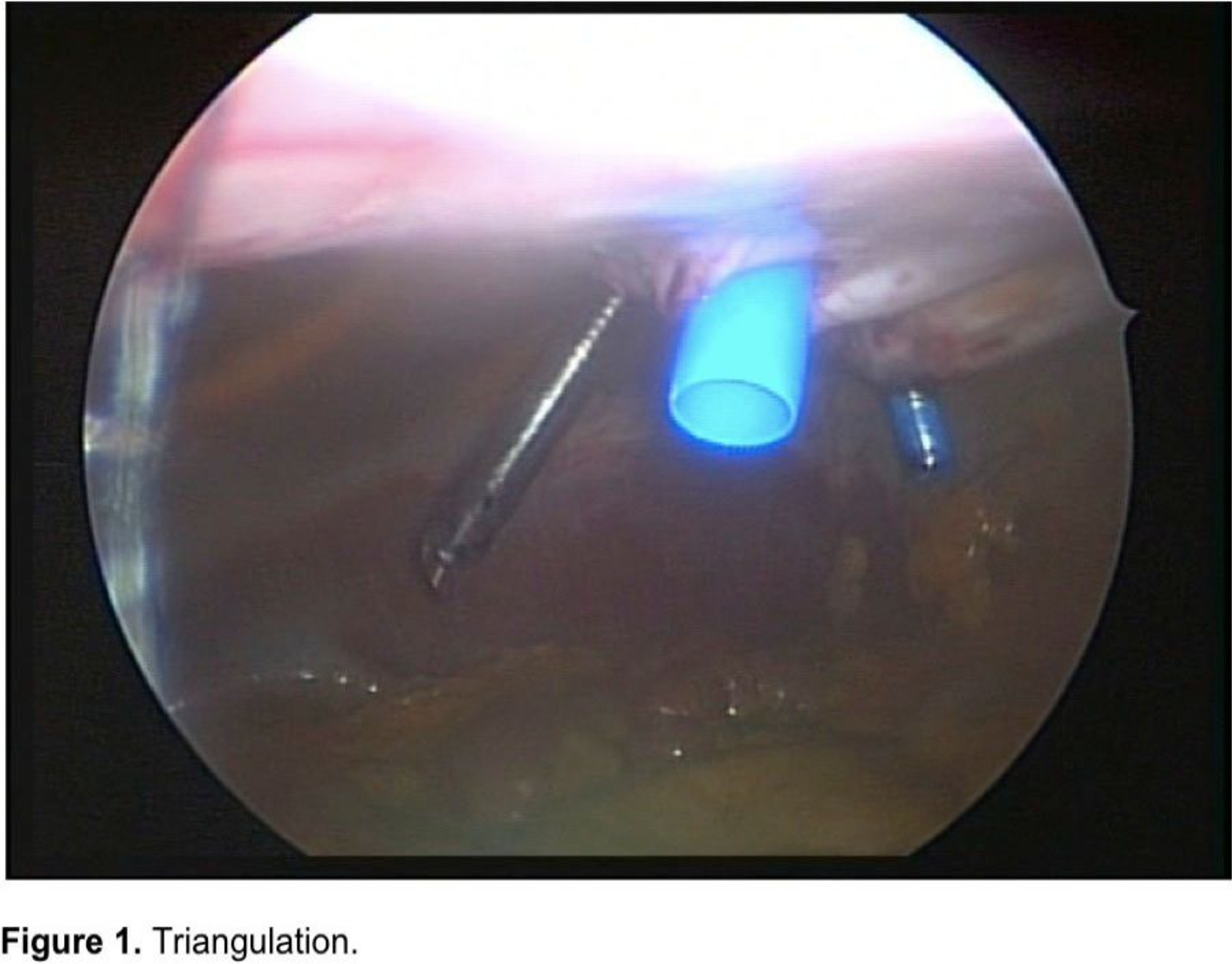
By spacing trocars at the abdominal wall, providing some triangulation, the axial view can be improved (Figure 1).
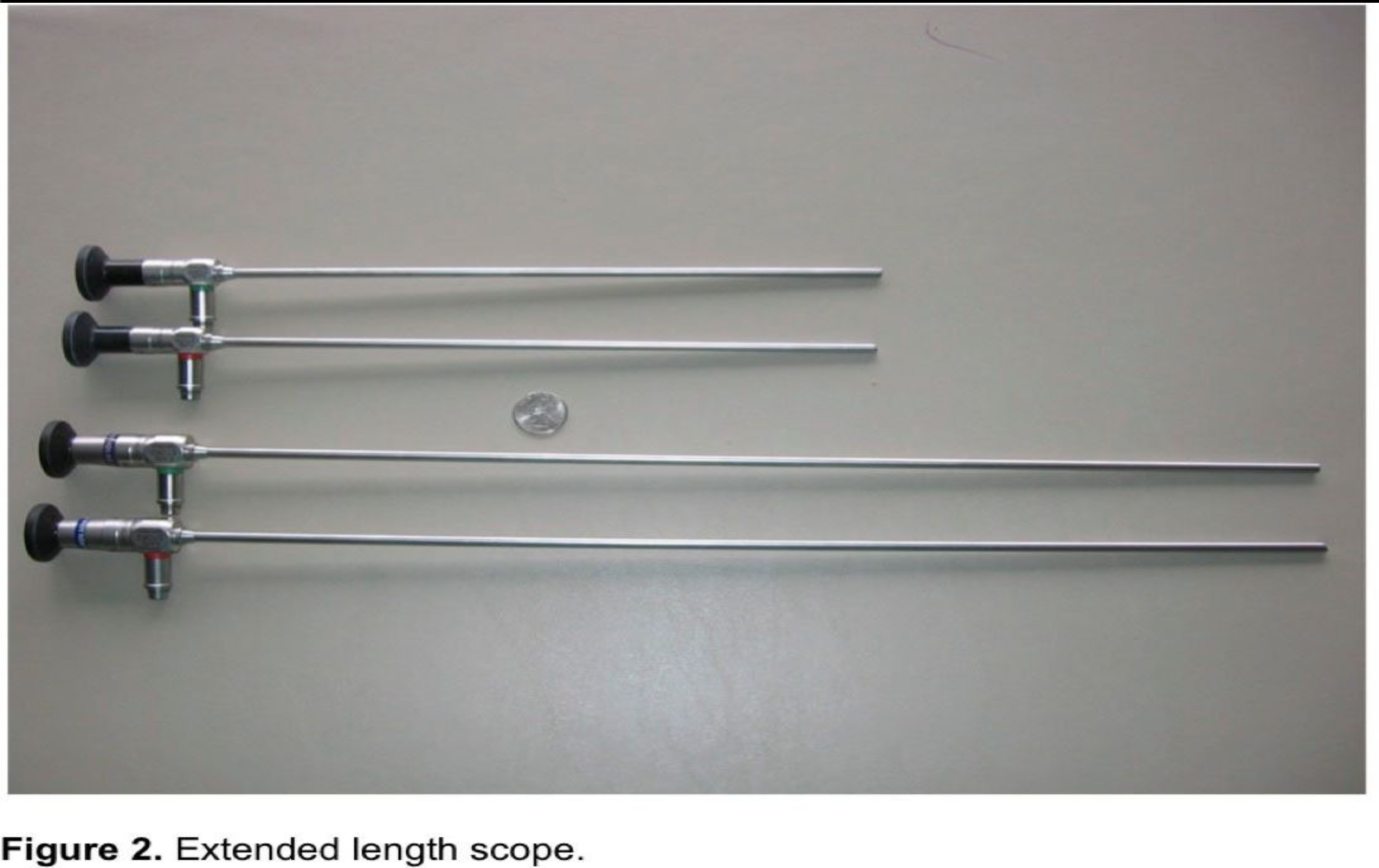
Standard and available scopes can be used with all reduced-port techniques. Typically, standard 5-mm laparoscopes are utilized. The 0º, 30º, or 45º scopes can be used. The angled scopes (30° and 45°) are more helpful as the instruments, and often the dissection, are in line with the scope. Extended length scopes are useful in reducing the clashing of primary surgeon and assistant’s hands by moving the camera head further back in the field (Figure 2). Flexible endoscopes can actually move the head of the camera completely out of the field, and work in this arena is progressing. Scopes with the light source extending from the back of the device also minimize the crowding of equipment. A right-angle adapter can actually be used if the light attachment exits from the side of the scope. Another option is flexible or articulating scopes that allow the end of the scope to flex or bend, thus enabling the view to reproduce the multiport approach. These scopes may also assist in insertion of subsequent trocars by retroflexing back to the abdominal wall.
The variable view scope, by use of a prism, allows the image to rotate from 0° to 120° without the end of the scope moving. Flexible endoscopes have been used also. These scopes present a promising future of enhanced visualization. They are, however, associated with a learning curve and require future development and improvement.
Instrumentation
Trocar devices that have been routinely used in multiport laparoscopy will need to be revisited. The focus over the past 20 years has been the shaft size (10mm to 5mm). The head of the trocar has made very little difference. Now, we are seeing the emergence of very-low profile single trocars and sleeves for single-port surgery (Figure 3).
Maintaining the head of the trocar at <2cm minimizes the collision of heads when placed in such close proximity. Both have advantages and disadvantages and should be evaluated before implementation.

Standard instrumentation can be used in almost all cases. Alternately, articulating or roticulating instruments may be useful in achieving triangulation. These may be associated with a learning curve.
New designs in instrumentation, such as bent or curved instruments, are emerging. These are designed to reduce the chopstick effect created by having multiple instruments in close proximity. Still in the initial stages, these instruments will need further study and proof of concept.
Exposure/Dissection
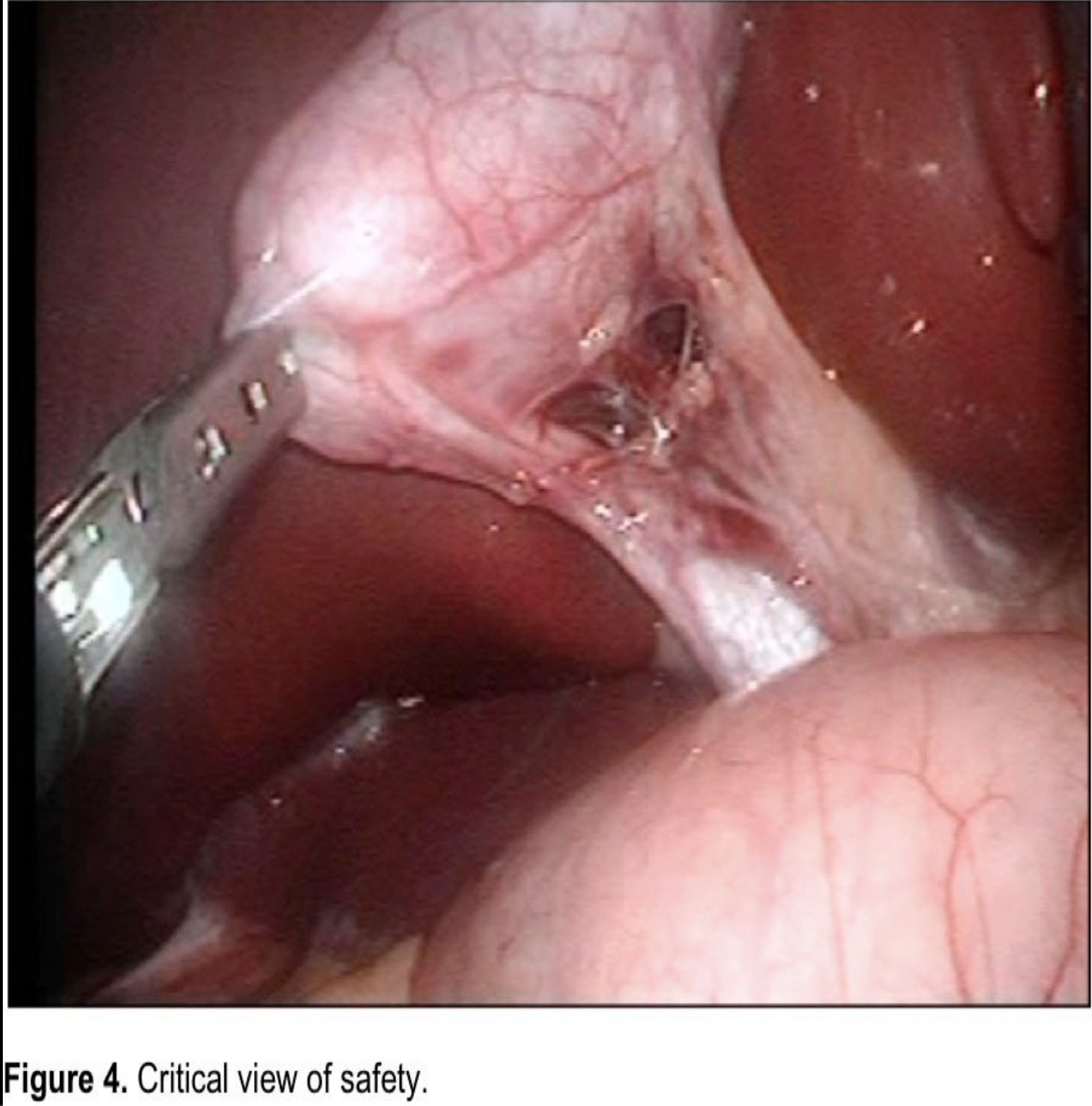
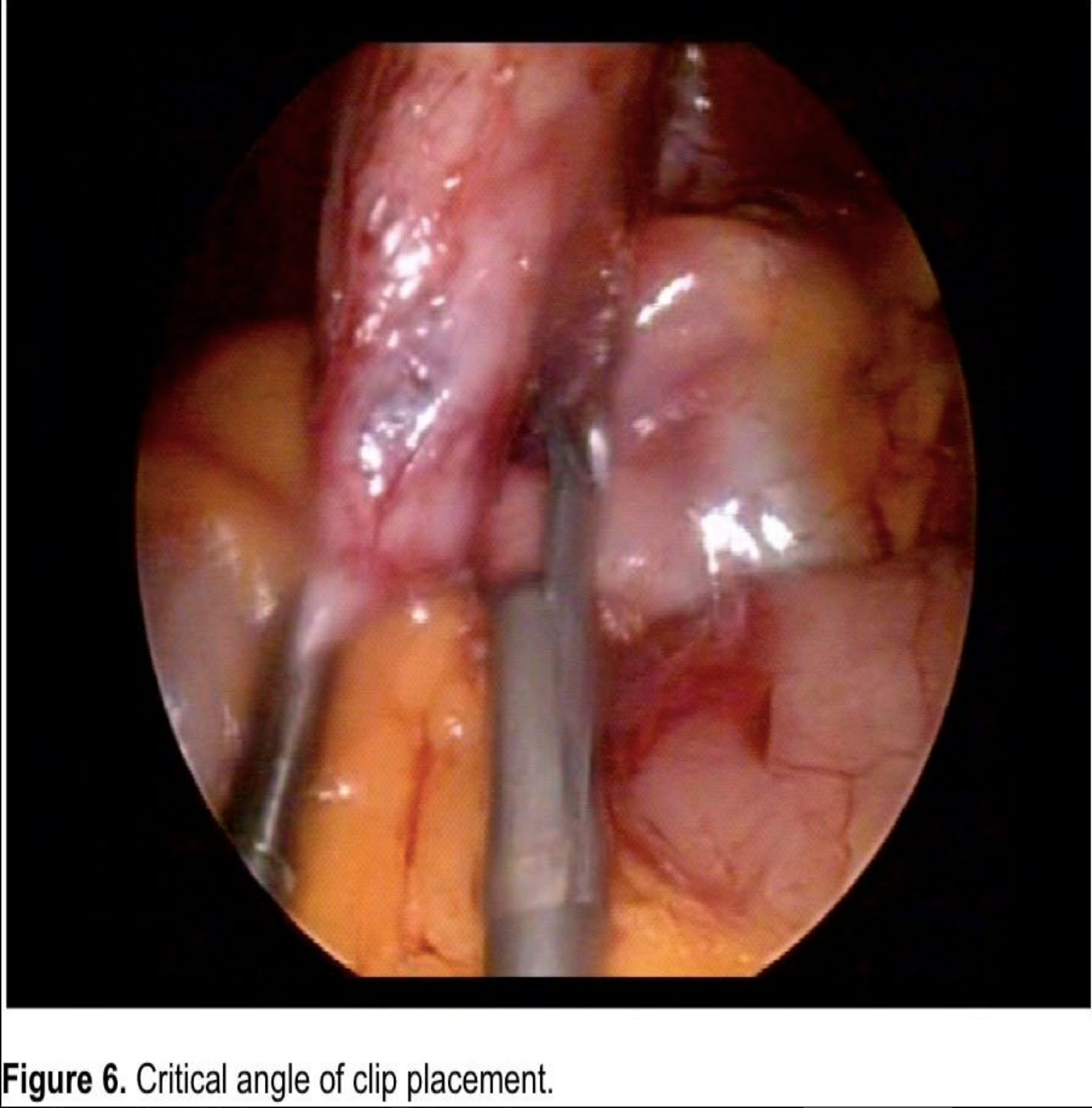
In many cases, single-access techniques reduce the number of instruments used in multiport procedures. Access devices typically have 3 channels, 1 visual and 2 operative. This may provide suboptimal retraction. Adding a transfascial retractor without a trocar left in place for the entirety of the case provides additional exposure. This is necessary, for example, when performing cholecystectomy. Without the additional retractor, it is difficult to achieve and maintain the critical view27 provided by independent fundal retraction and infundibular manipulation (Figure 4, 5a, 5b). In addition, the critical angle of clip placement (Figure 6), described as placement of the clip perpendicular to the cystic duct, may not be possible. This is easily attained in multiport cholecystectomy as the clip applier enters from the subxyphoid port and is already in the perpendicular position to the duct but becomes more difficult in single-port access, and care must be taken to not place the clip tangentially to avoid possible cystic duct stump leak.
Improvements in adding the fourth site of entry in access devices and techniques are being developed with 4 channels to combat this problem.
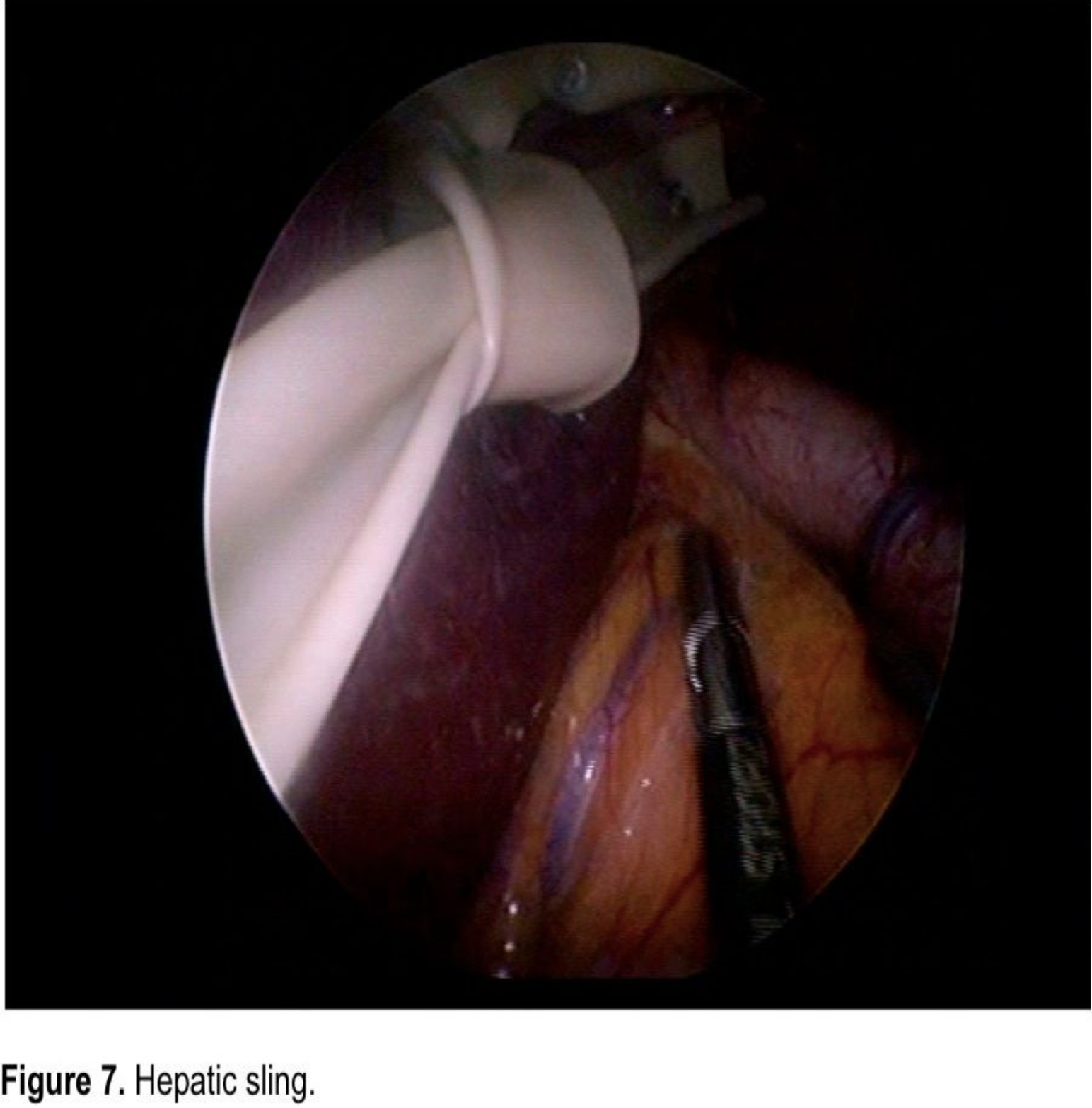
Novel exposure techniques also exist. Transabdominal sutures may be placed to provide somewhat dynamic retraction. Intraabdominal techniques, such as the hepatic sling28 where the liver is retracted with Penrose drains tacked to the abdominal wall, may be used (Figure 7). In some techniques, a liver retractor may be placed directly through the skin. Creation of triangulation may be achieved first, by creating distance at the abdominal wall, and second, if needed, by using articulating instruments. A promising area of retraction may be the use of magnets being developed at several institutions.
We must be cautious, however, as we apply new ideas of techniques. Simply placing a needle and suture may seem benign, but perforation of the gallbladder may have undesirable results. Aside from manipulation of a sharp instrument within the abdominal cavity and bile spillage, concerns have been raised with respect to effects on possible malignancies.29,30 This concern would also leave some retraction techniques as unusable alternatives in some procedures (ie, ovarian cancer, colon procedures, and retraction of bowel in adhesiolysis or hernia repair).
Abdominal Closure
Even in multiport laparoscopy, trocar sites have been studied, because they may result in hernia formation. Several studies have already demonstrated the increased risk of hernia formation with larger trocars. The progression from 5-mm to 10-mm to 15-mm trocars has seen an increased incidence of ASH. As we introduce larger single-port devices, we must be cautious not to predispose the patients to the known risk of increased hernia formation with the larger incision often approaching 3cm.
Although 5-mm trocar sites are not typically closed in multiport procedures, each fascial defect should be oversewn. In many cases, the fascial trocar entry sites are joined to facilitate organ removal. In this case, a single running stitch may be used to close the defect. If using an access device, the single defect should be reapproximated.
All skin incisions should be reapproximated (Figure 8).
Rescue Strategies
An integral aspect of single-port surgery is single-port rescue. All patients should be informed and consented for conversion possibilities including addition of port sites or open procedures. If adequate visualization cannot be achieved via the single port, adding trocars either within the single incision or at a distant site on the abdominal wall may provide better exposure. Adding retractors without trocars to be left for the entirety of the case may also be an option.
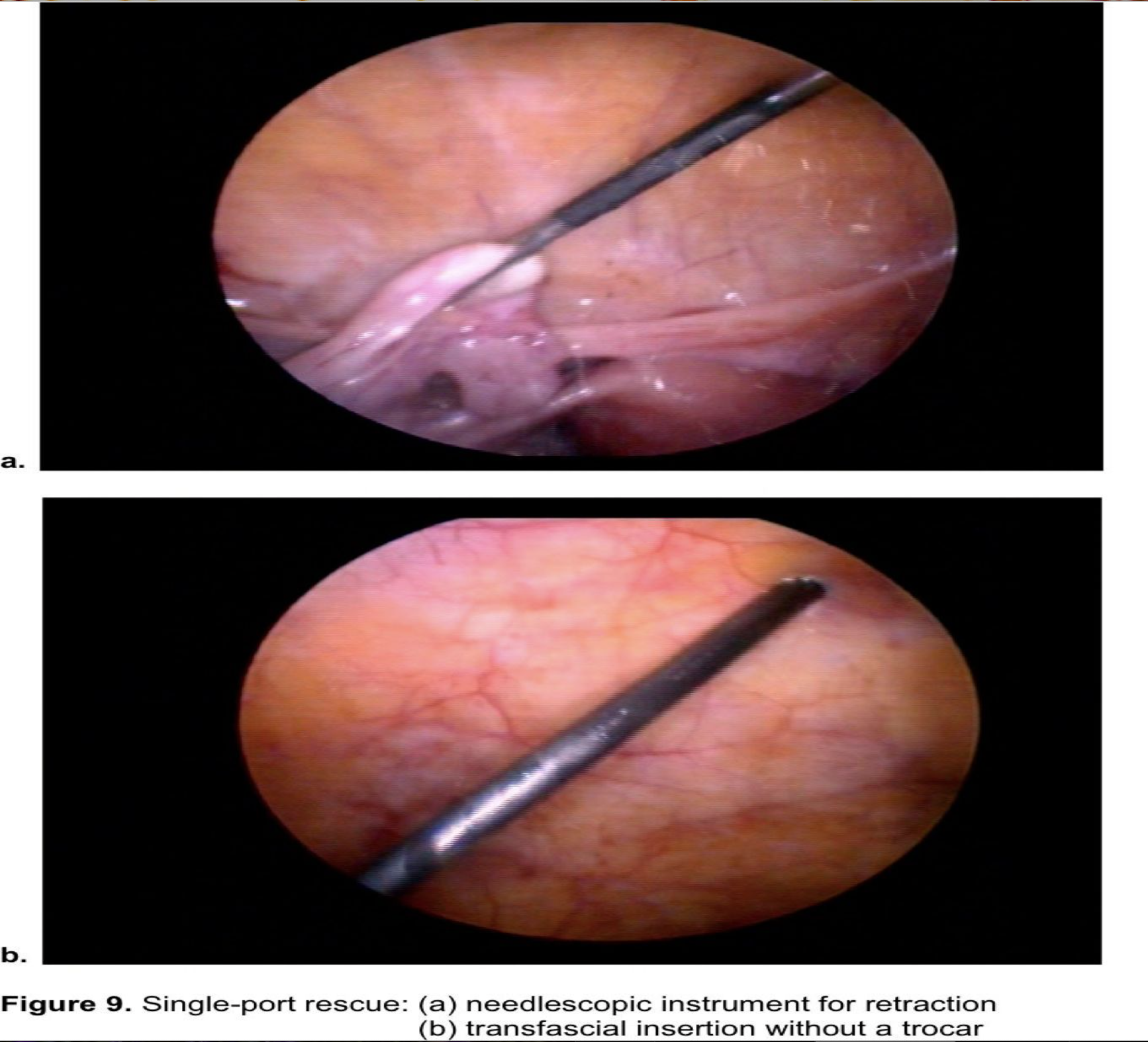
The concept of reduced-port surgery, unlike the dictum of single-port surgery, would prompt one to simply reduce the number or “size” of the incisions. With this philosophy, the already proven platform of needlescopic instrumentation (Figure 9) is a viable alternative. Even though the procedure may not be completed with only a single-port approach, one may be able to accomplish a reduced-port procedure in a safe fashion with the desired cosmetic benefit.
As with multiport laparascopy, we must always focus on adequate exposure, dissection and correct identification of anatomy. Thus, indications for conversion to open are the same as for multiport laparoscopy.
Follow up/Complications
Postoperative care and follow-up mirrors that of multiport laparoscopy. Any benefits of decreased length of stay, decreased narcotic requirements or pain, or faster return to activities of daily living have yet to be proven.
The incision must be evaluated in the immediate postoperative setting and in the long term. Maintaining a clean, dry dressing or skin site to avoid infection is important. The potential for seroma formation is increased with the creation of the skin flaps. Also, given that we are now placing larger access devices or more trocars through a single incision, care must be taken to ensure that healing occurs without wound breakdown. Whether these techniques may actually lend themselves to increased pain secondary to the increased manipulation at these sites will need to be determined.
Long-term follow-up for access site hernias (ASH) is crucial. In the practice of multiport laparoscopy, defects >5mm are typically closed as the risk of hernia formation increases with increasing incision size.31,32 The effect of multiple fascial defects in close proximity is unknown, and, therefore, all individual defects should be closed. Larger access devices requiring an approximate fascial defect of 2cm should be carefully closed. We will need to continue to follow the access sites and consider this. After all, if the primary benefit is going to be cosmetic, an increased rate of hernia formation could negate any cosmetic benefit.
CONCLUSION
Reduced-port surgery has seen rapid growth and adoption over the past 2 years. Compared with NOTES, the properties that make it more readily available may also be their most concerning risk. NOTES has an almost “built in” safety net with the expense, IRB requirements, and technical difficulties. Although these factors may slow the progression of NOTES, they help maintain the integrity and safety. Reduced-port techniques can be less costly, may be permitted without IRB, and are technically easier to perform. Although this will enhance adoption, the “safety net” has been removed.
Performing laparoscopic procedures via a single portal is an alternative to multiport procedures. Although these 2 platforms are similar, relying on many of the same basic principles and instrumentation, differences do exist. Recognizing these differences will eliminate potential pitfalls and aid in the development of this novel technique and future technology.
Entry into this field should be deliberate and well thought out. To go directly from 4 or 5 port sites to one overnight can be difficult and may involve too many new techniques, such that the learning curve may become unnecessarily steep. Rather, a progression from multiple port sites to a single site will allow surgeons to “successfully” reduce the port sites to a level with which they are comfortable. Thus, by gradually decreasing access sites, final consolidation at a single port may result in a smoother transition and more reproducible outcomes. On the other hand, the idea of reduced-port surgery may have a goal of 2 incisions in some procedures rather than always focusing on one.
Whether reduced-port surgery is going to be the next step toward NOTES, develop into a platform of its own, or lead us down a path we have not yet realized will certainly become apparent over the next few years. Whichever direction we go in, the driving force needs to be patient safety and patient care.
Address correspondence to: Paul G. Curcillo II, MD, Vice Chairman, Department of Surgery, Director, Robotics and Minimally Invasive Surgery, 219 North Broad Street, 10th Floor, Philadelphia, PA 19107, USA. Telephone: (215) 762-5577, Fax: (215) 762-5588, E-mail: pgc@curcillo.com
References
- de la Fuente SG, Demaria EJ, Reynolds JD, Portenier DD, Pryor AD. New developments in surgery: Natural Transluminal Endoscopic Surgery (NOTES). Arch Surg. 2007 Mar;142(3):295-297.
- Navarra G, Pozza E, Occhionorelli S, et al. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695.
- Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361-364.
- Kalloo AN, Singh VK, Jagannath SB, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114-117.
- Curcillo PG, Podolsky ER, Rottman SJ. Single port access (SPA) cholecystectomy. Gastroenterology. 2008;134:A-858.
- Podolsky ER, Rottman, SJ, King SA, Curcillo PG. Single port access (SPA™) cholecystectomy. Surg Endosc. 2008;22(Suppl 1). DOI: 1007/s00464-008-9821-3.
- Bessler M, Stevens PD, Milone L, Hogle NJ, Durak E, Fowler D. Multimedia article: Transvaginal laparoscopic cholecystectomy: laparoscopically assisted. Surg Endosc. 2008;22(7):1715-1716.
- Gumbs AA, Fowler D, Milone L, Evanko JC, Ude AO, Stevens P, Bessler M. Transvaginal natural orifice translumenal endoscopic surgery cholecystectomy: early evolution of the technique. Ann Surg. 2009;249(6):908-912.
- Rao PP, Bhagwat SM, Rane A, Rao PP. The feasibility of single port laparoscopic cholecystectomy: a pilot study of 20 cases. HPB. 2008;10(5):336-340.
- Tacchino R, Greco F, Matera D. Single incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009;23:896-899.
- Nguyen NT, Reavis KM, Hinojosa MW, Smith BR, Wilson SE. Laparoscopic transumbilical cholecystectomy without visible abdominal scars. J Gastrointest Surg. 2009;13:1125-1128.
- Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010 Jun;24(6):1403-1412. Epub 2009 Dec 25.
- Binenbaum SJ, Teixeira JA, Forreste GJ, et al. Single-incision laparoscopic cholecystectomy using a flexible endoscope. Arch Surg. 2009;144(8):734-738.
- Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009 Jul;23(7):1419-1417. Epub 2009 Apr 4.
- Strasberg SM, Hertl M, Soper NJ. Analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101-105.
- Olsen D. Bile duct injuries during laparoscopic cholecystectomy. Surg Endosc. 1997; 11:133-138.
- Rossi RL, Schirmer WJ, Braasch JW, et al. Laparoscopic bile duct injuries: risk factors, recognition, and repair. Arch Surg. 1992;127:596-602.
- King SA, Atogho A, Podolsky ER, Curcillo PG. Single port access (SPA) bilateral oopherectomy and hysterectomy. Laparoscopy Today. The Green Issue. 2008;7;2,26
- Castellucci SA, Curcillo PG, Ginsberg PC, Saba S, Jaffe J, Harmon JD. Single port access adrenalectomy. J Endourol. 2008;8;1573-1576.
- Poor A, Podolsky ER, King SA, Curcillo PG. Single port access (SPA) colon resection [abstract 8358]. JSLS. 2008;12(3 Suppl):S70.
- Podolsky ER, Curcillo PGC. Single Port Access (SPA) surgery: a 24 month experience. J Gastrointest Surg. 2009. DOI 10.1007/s11605-009-1081-6.
- Curcillo PG, King SA, Podolsky ER, Rottman SJ. Single port access (SPA™), minimal access surgery through a single incision. Surg Tech Int. 2009;18:19-25.
- Podolsky ER, Rottman SJ, Curcillo PG 2nd. Single port access surgery (SPA) gastrostomy tube in patients unable to receive percutaneous endoscopic gastrostomy placement. Surg Endosc. 2009 May;23(5)1142-1145. Epub 2009 March 5.
- Podolsky ER, Curcillo PG. A Comparison of Independence of Motion in Single Port Access Techniqes. Surg Endosc. 2010; 24: S499. DOI 1007/s00464-010-0972-7
- Podolsky ER, Curcillo PG. Single Port Access Surgery: Evaluation of Access Platforms, Versatility and Fascila Defects. Surg Endosc. 2010; 24: S639. DOI 10.1007/s00464-010-0972-7
- Curcillo PG, King SA, Podolsky ER, Mouhlas A, Poor A, Wu A. Single port access (SPA) surgery technique using a novel laparoscopic single incision approach. (online video and abstract) Surg Endosc. Epub October 2009
- Podolsky ER, Curcillo PG. Reduced port surgery: preservation of the critical view in SPA cholecystectomy. Surg Endosc. Epub May 2010
- Podolsky ER, Naziri W, Curcillo PG. Single port access (SPA) gastric band placement. Bariatric Times. 2009;6(6):29-31.
- Bucher P, Pugin F, Morel P. Laparoendoscopic single site surgery and occult gallbladder cancer. Surg Endosc. 2010 Jul;24(7):1791-1792.
- Gibbs KE, Kaleya RN. Incidental gallbladder cancer and laparoscopic single incision cholecystectomy. Surg Endosc. 2009;23:1680.
- Boughey JC, Nottingham JM, Walls AC. Richter’s hernia in the laparoscopic era: four case reports and review of the literature. Surg Laparosc Endosc Percutan Tech. 2003 Feb;13(1):55-58.
- Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M. Trocar site hernia. Arch Surg. 2004;139:1248-1256.
